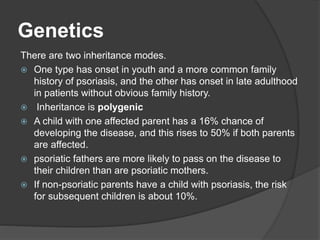
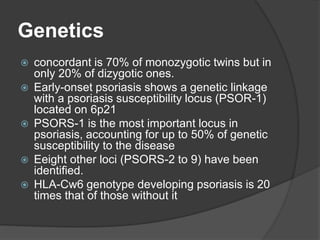
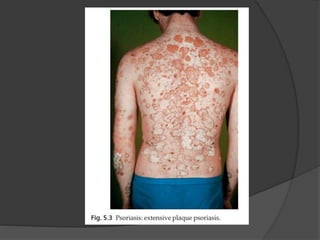
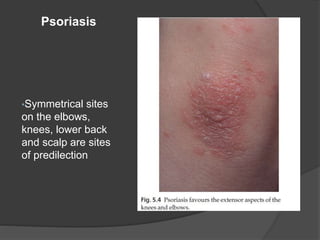
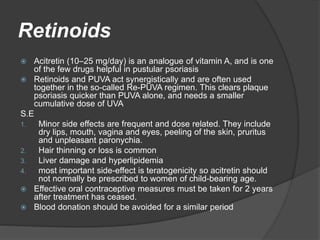
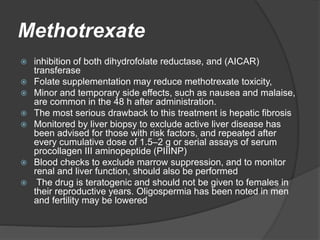
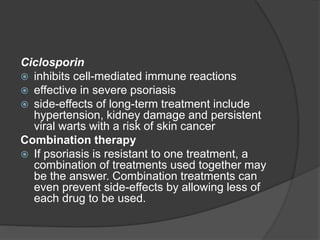
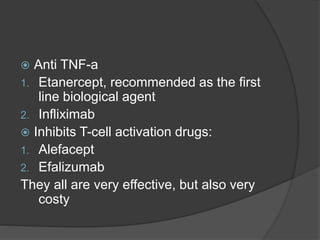
Psoriasis is a chronic skin condition characterized by inflamed plaques and scales. It affects 1-3% of populations and has a genetic component. The causes involve an immune reaction and abnormal skin cell growth. Symptoms range from small red spots to widespread inflammation. Treatments include topical creams and light therapy. For severe cases, oral medications like retinoids, methotrexate and biologics may be used. Psoriasis has no cure and requires long-term management of symptoms.