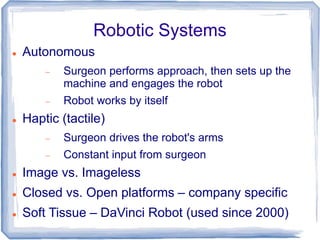
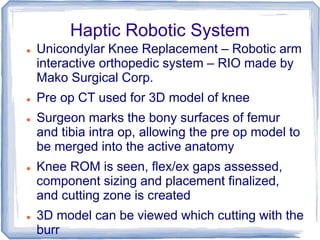
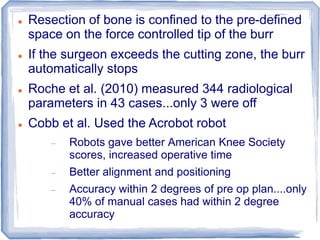
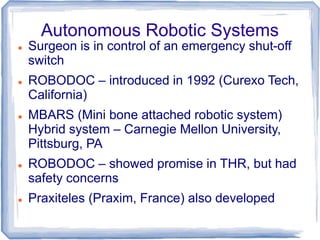
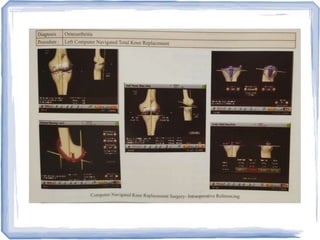
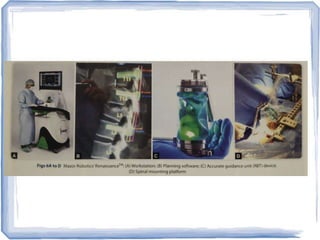
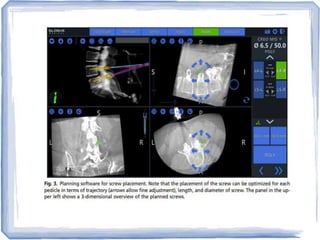
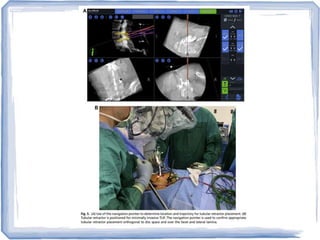
This document discusses the use of robots in orthopaedic surgery. It describes how robotic systems can improve accuracy of bone cuts and component placement compared to manual surgery. Both autonomous and haptic robotic systems are presented. Applications discussed include unicondylar knee replacement using the Mako robotic arm and spinal pedicle screw placement using the Renaissance system. While robotic surgery may provide benefits like increased accuracy, it also has drawbacks such as high costs and long-term outcomes have not proven superiority over manual techniques.