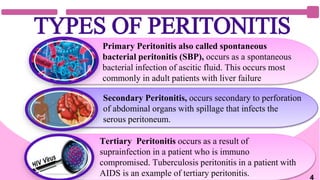
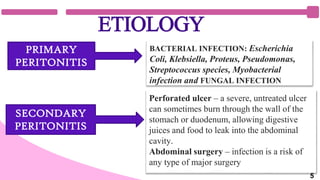
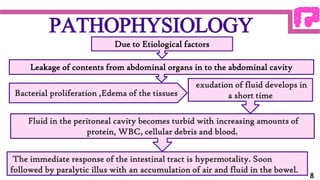
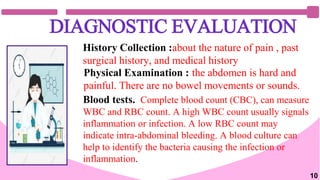
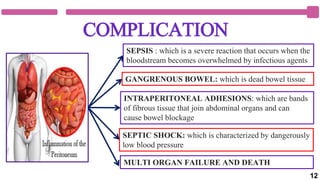
Peritonitis is an inflammation of the peritoneum caused by bacterial or fungal infection. Left untreated, it can lead to sepsis, multiple organ failure and death. There are three main types: primary occurs spontaneously with liver failure; secondary follows a perforation of abdominal organs; tertiary occurs in immuno-compromised people like with AIDS and tuberculosis. Symptoms include severe abdominal pain, fever, nausea and vomiting. Diagnosis involves medical history, exams, blood tests and imaging scans. Treatment requires intravenous fluids, antibiotics, pain relief, and may require surgery to repair damaged organs and drain infections. With proper treatment outcomes are good, but risks include sepsis, adhesions and organ failure if not addressed promptly.