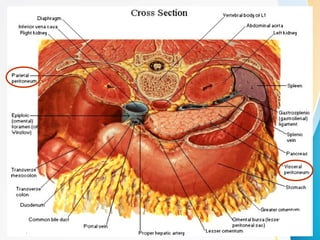
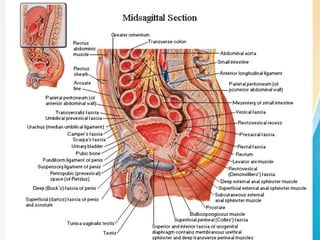
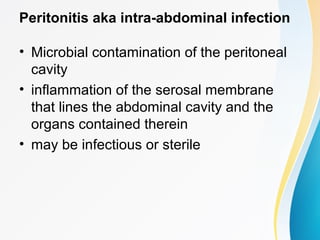
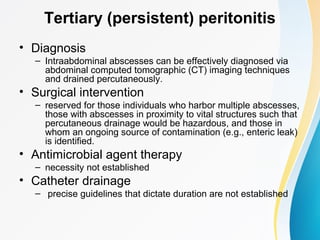
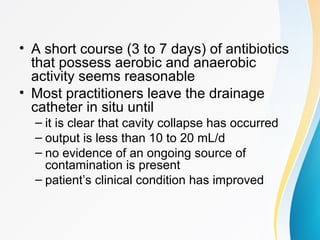
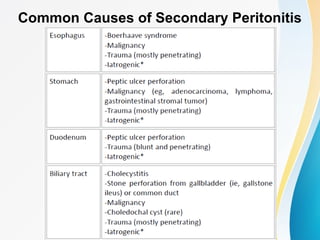
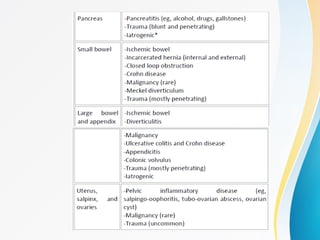
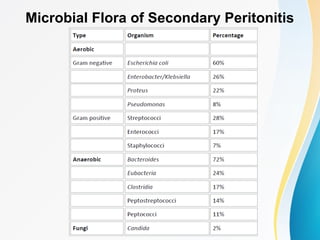
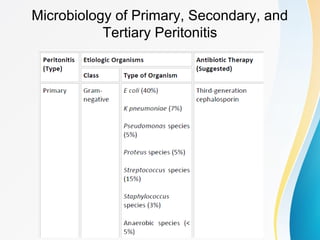
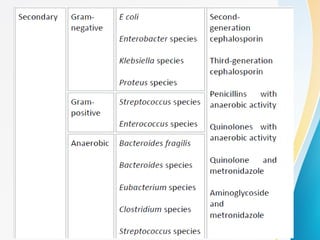
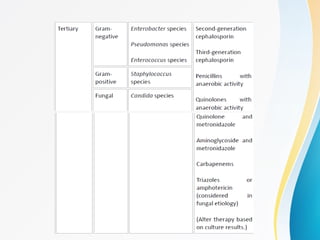
Peritonitis refers to inflammation of the peritoneum lining the abdominal cavity. There are three main types: primary involves direct bacterial invasion from the bloodstream; secondary occurs when the peritoneum is contaminated by a perforated organ; and tertiary develops in immunocompromised patients and is difficult to treat. Primary peritonitis involves a single bacterium and usually resolves with antibiotics alone. Secondary peritonitis requires source control through surgery in addition to broad-spectrum antibiotics to address mixed aerobic and anaerobic bacteria. Tertiary peritonitis has high mortality over 50% even with antibiotics and source control due to drug-resistant bacteria and weakened host defenses.