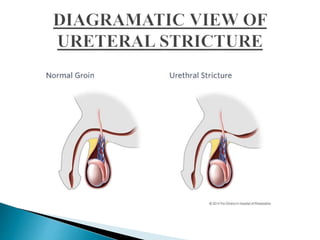
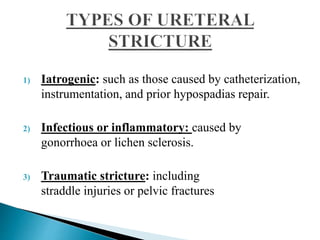
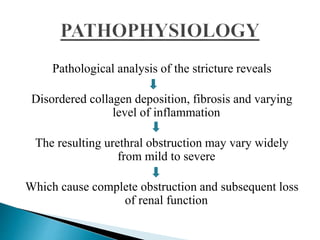
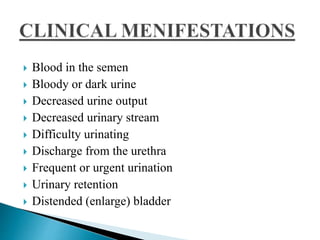
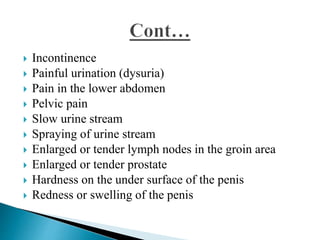
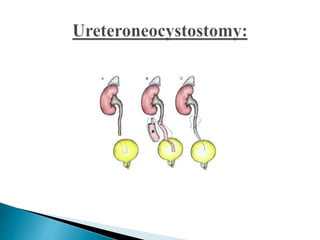
This document discusses urethral strictures, which are characterized by a narrowing of the urethral lumen causing obstruction. Common causes include ureteropelvic junction obstruction, pelvic radiation therapy, urinary diversion surgery, traumatic injuries, congenital anomalies, kidney stones, cancers, and infections. Symptoms include blood in urine or semen, painful urination, and decreased urine flow. Diagnosis involves examinations, urinalysis, imaging tests. Treatment options include balloon dilation, endoureterotomy, ureteral stents, transureteroureterostomy, and ureteroneocystostomy.