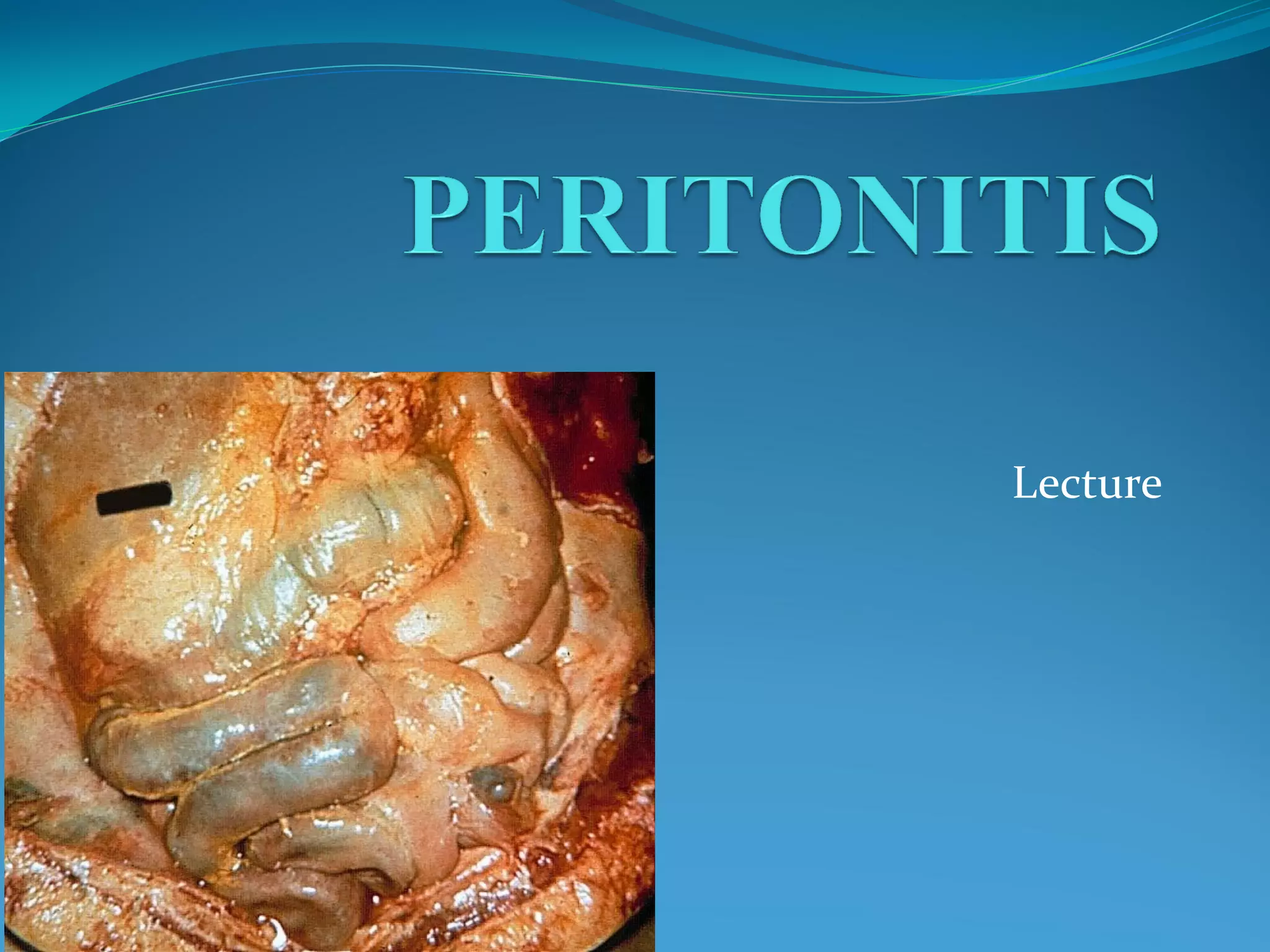
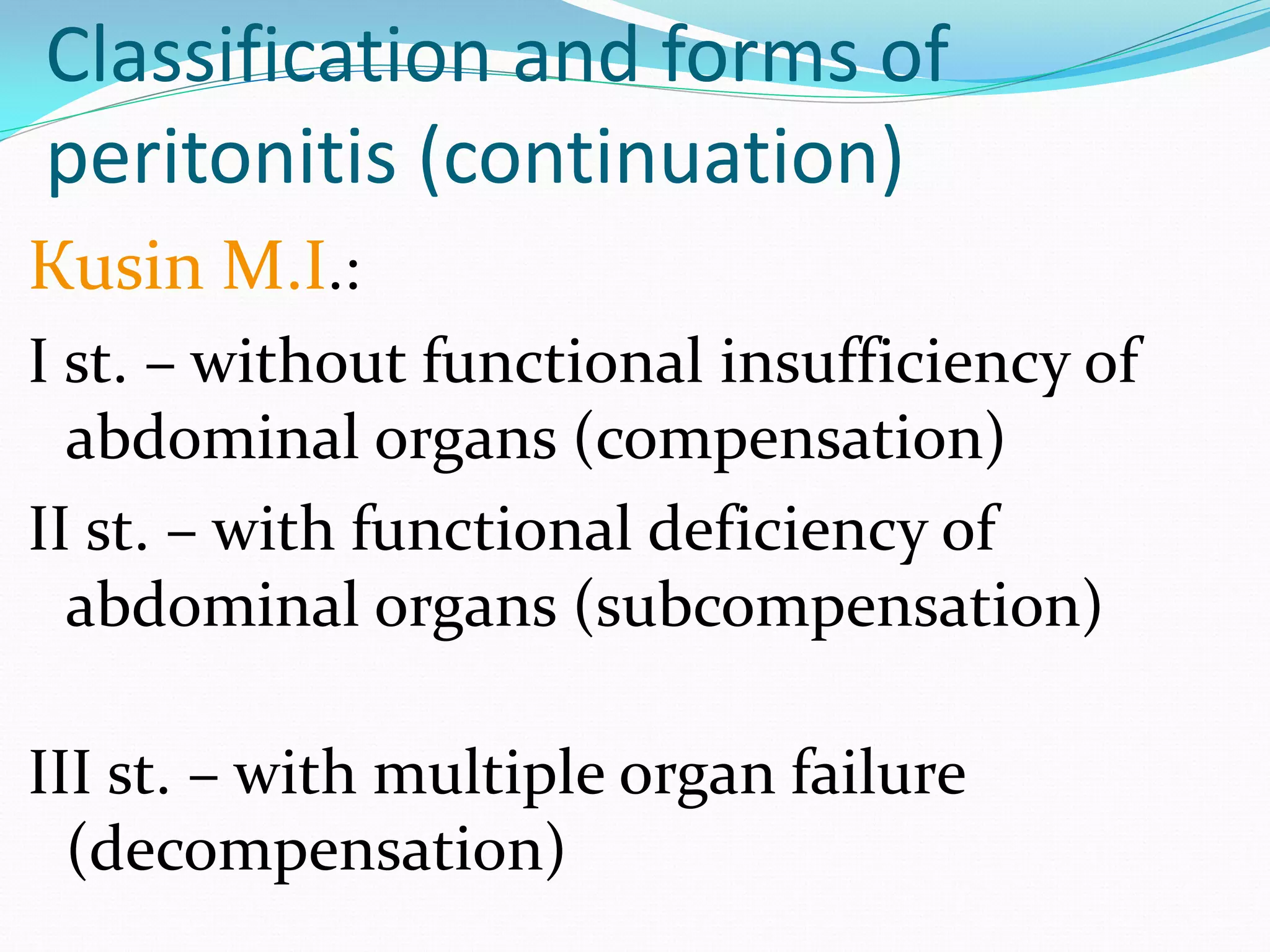
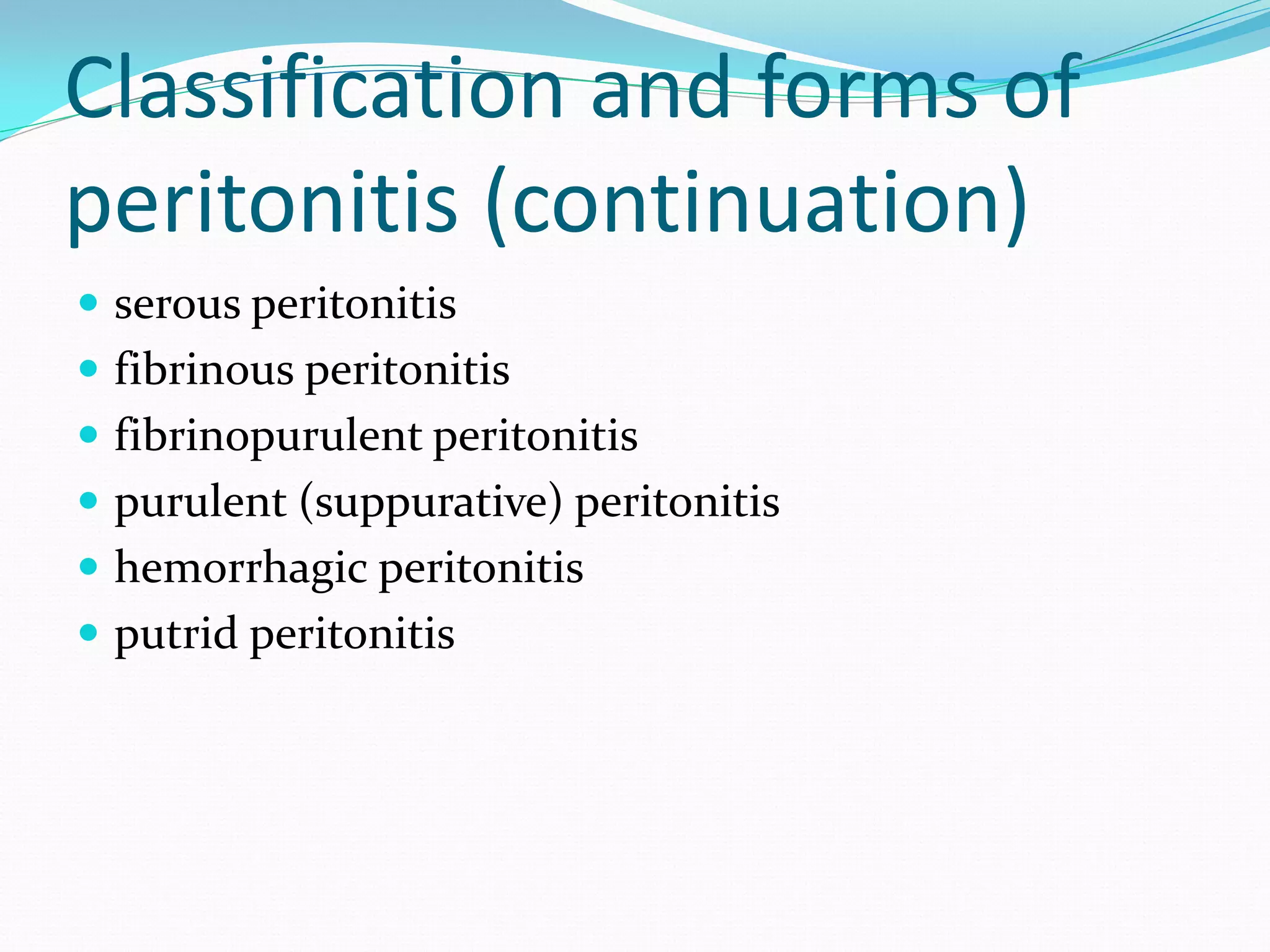
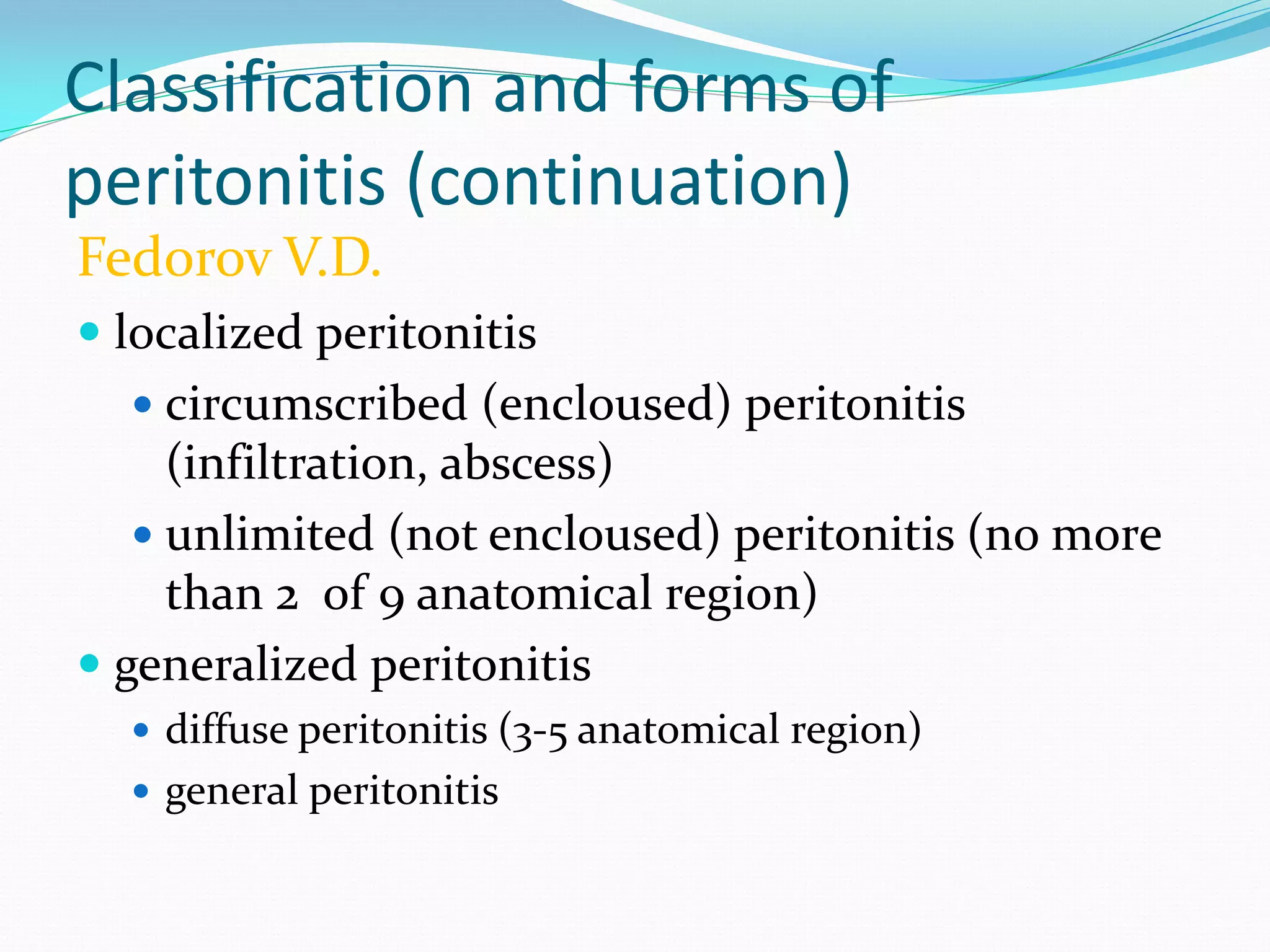
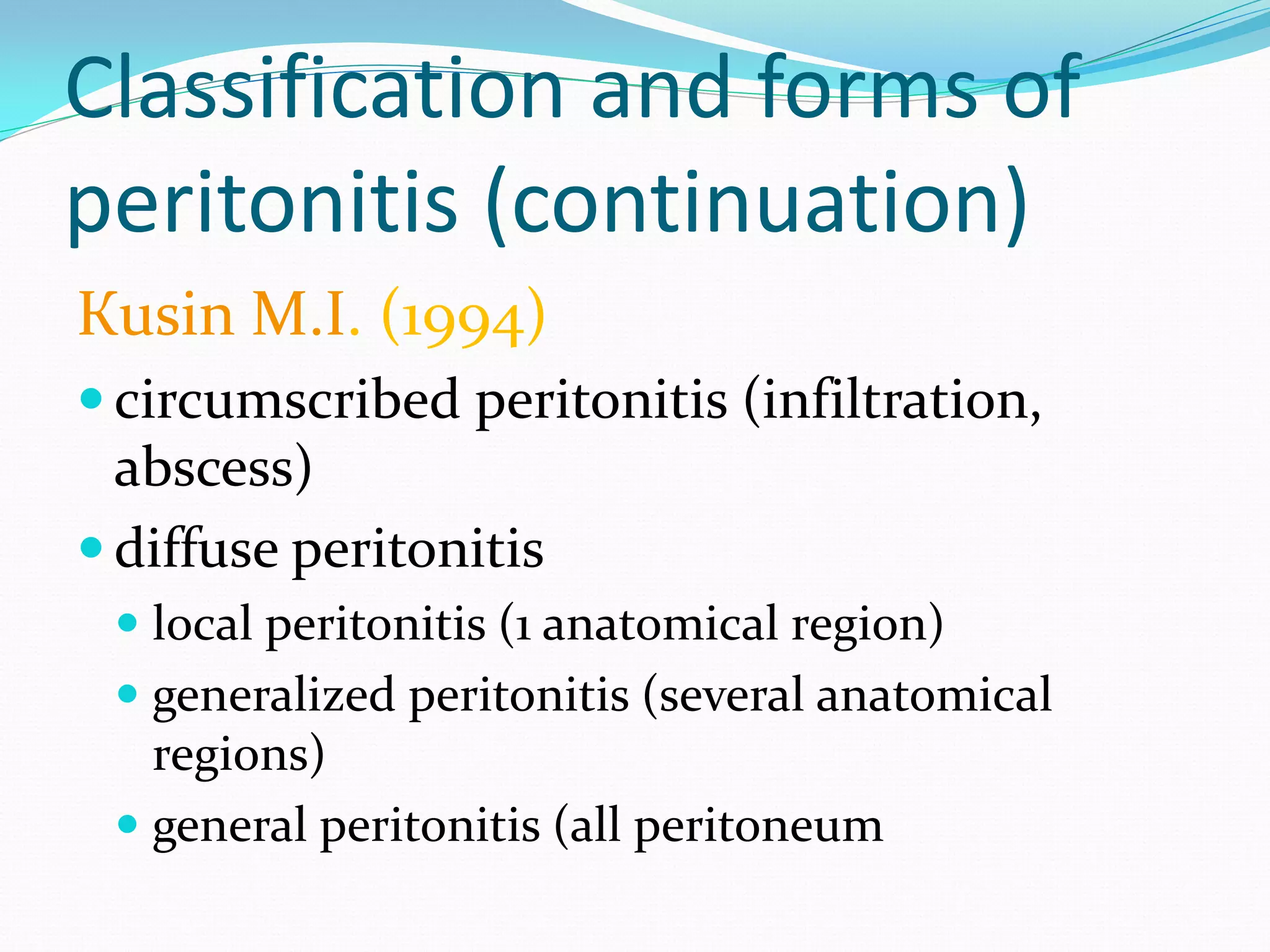
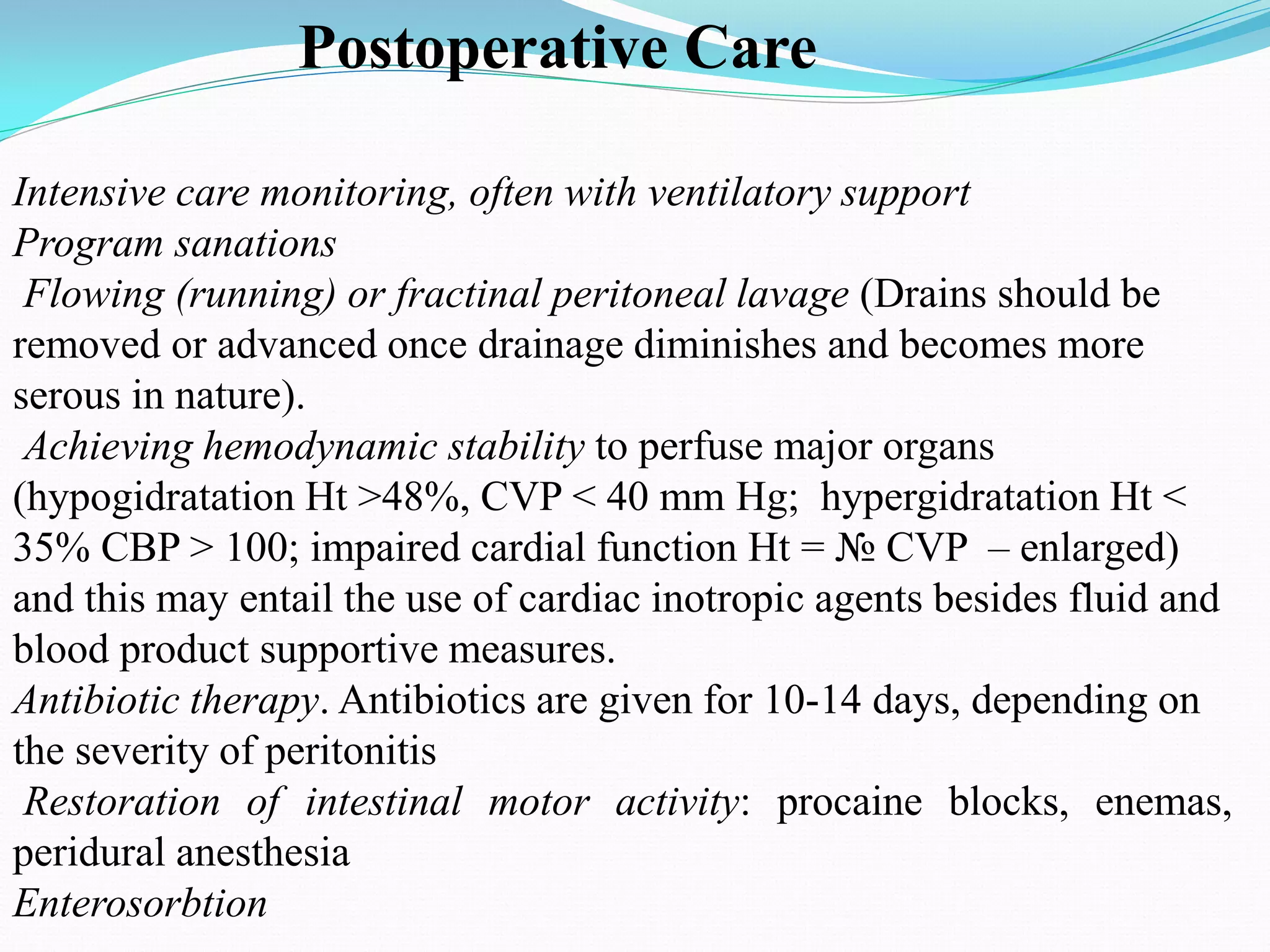
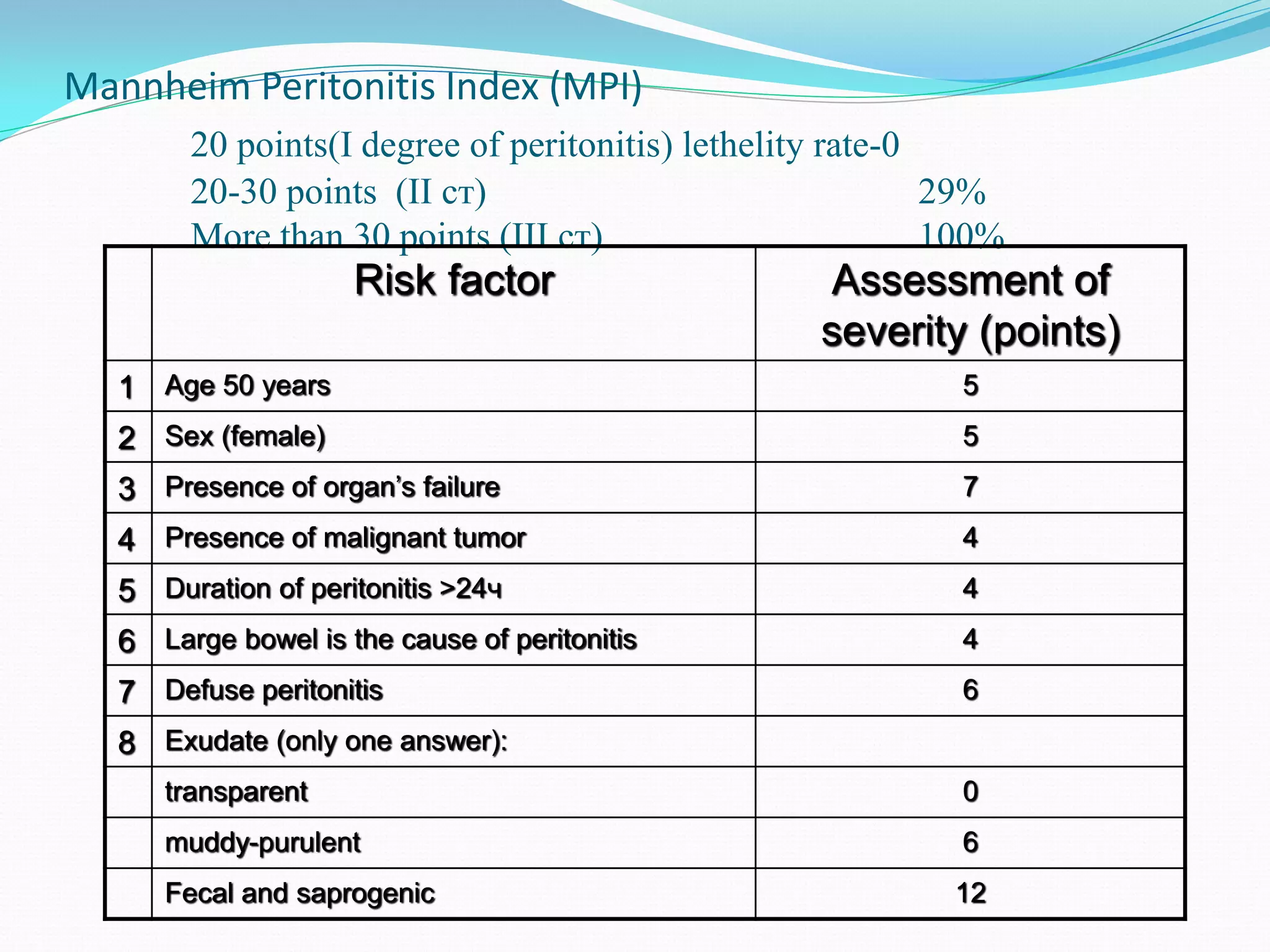
Peritonitis is inflammation of the peritoneum lining the abdominal cavity. It can be caused by infection, injury, or chemical irritation. Acute peritonitis requires prompt treatment to eliminate the infectious source and reduce bacterial load. Treatment involves intravenous antibiotics, surgery to resolve the underlying cause, and intensive care as needed. Prognosis depends on the severity and cause of peritonitis. More severe or generalized cases with organ dysfunction carry a high risk of complications and mortality.