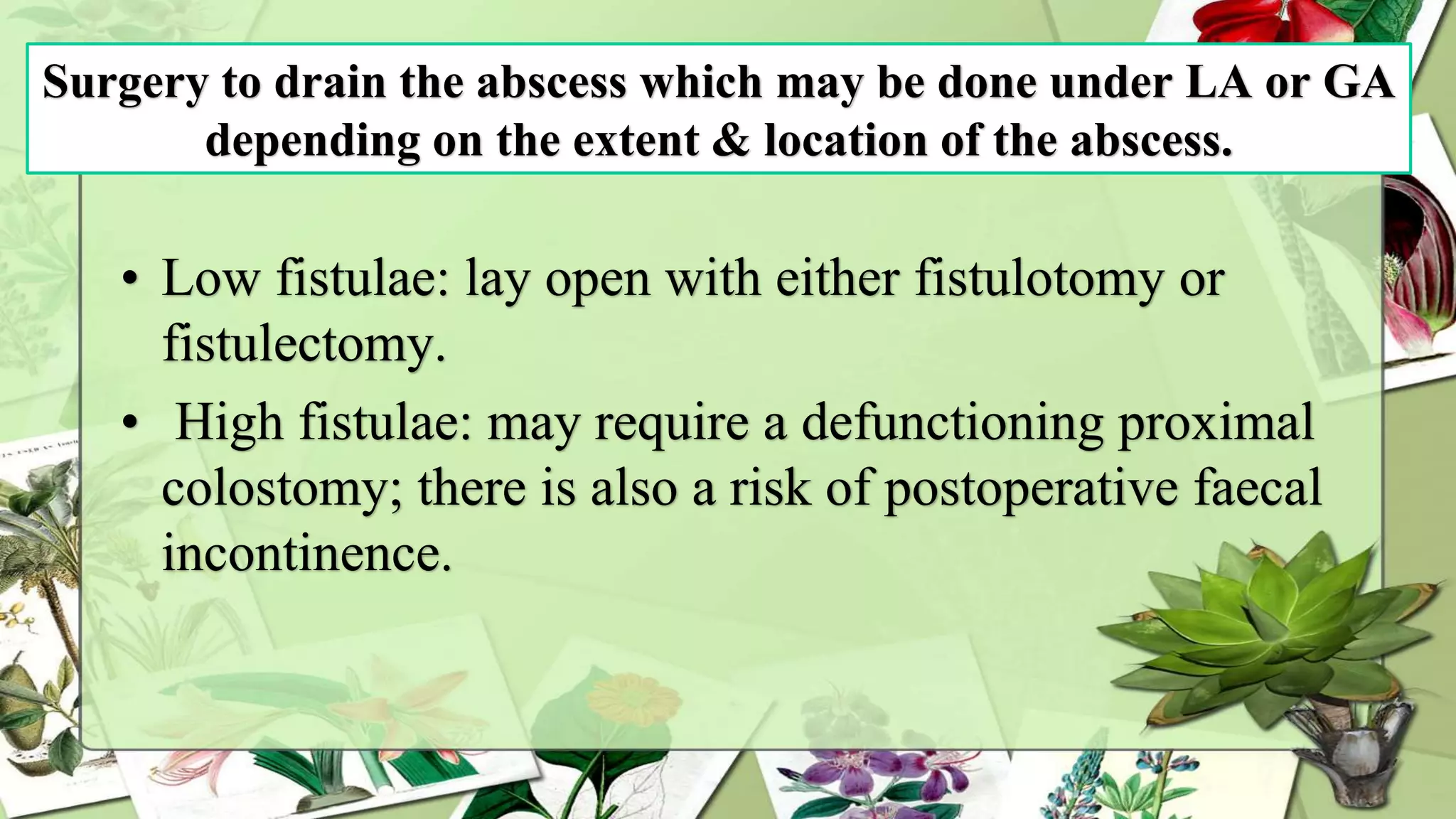
An anorectal abscess is a pus-filled infection in the anal or rectal region, often caused by anal fissures, STIs, or blocked glands. The condition presents with symptoms such as painful swelling, discharge, and fever, with prompt treatment leading to good recovery outcomes. Common types include perianal, ischiorectal, and intersphincteric abscesses, requiring diagnosis via digital examination and possibly imaging, with treatment typically involving surgical drainage.