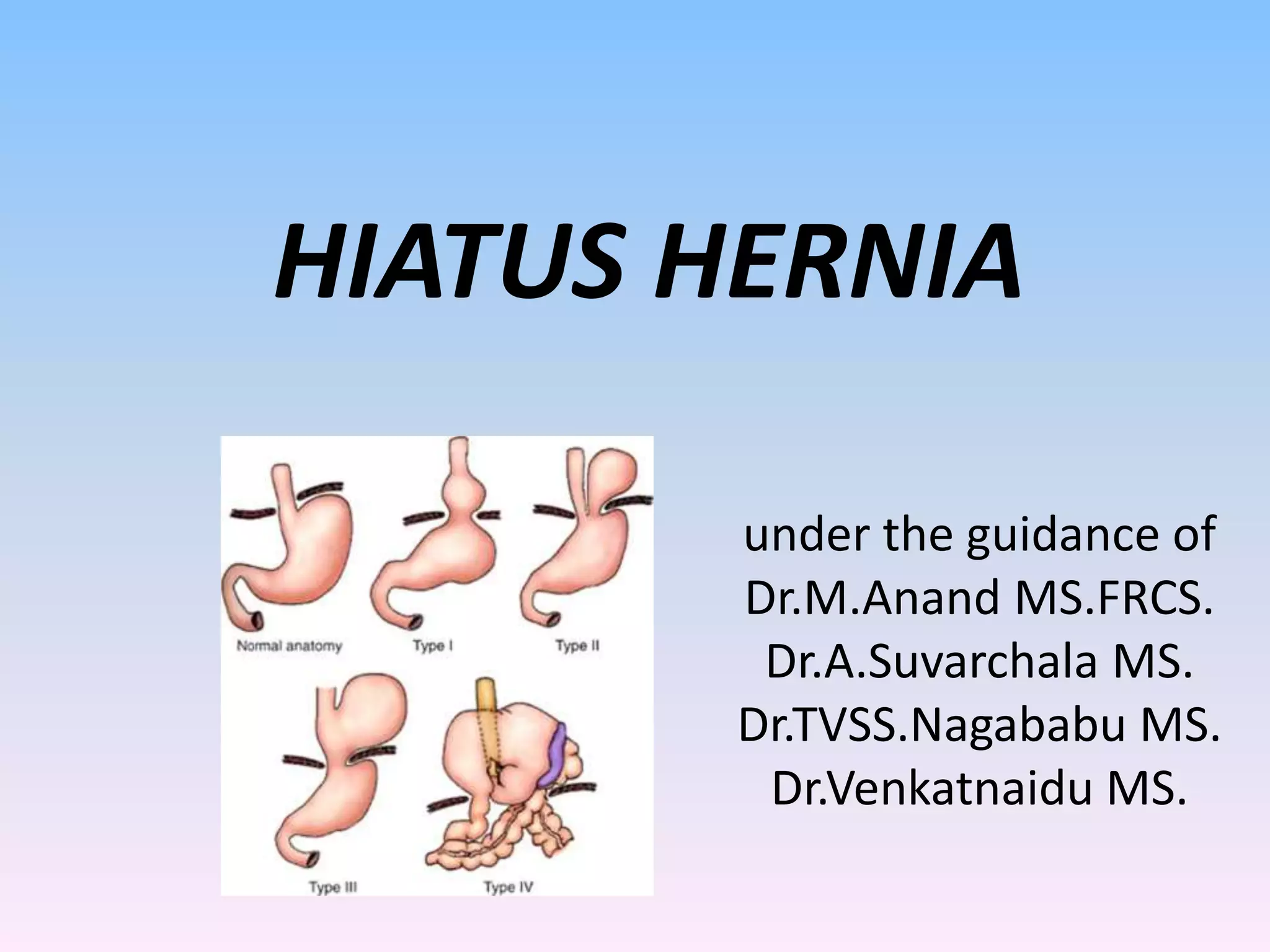
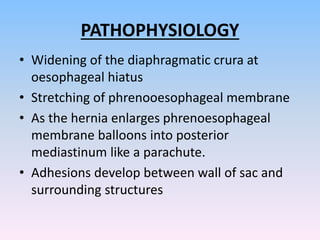
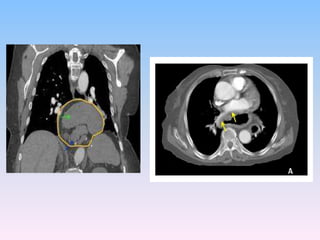
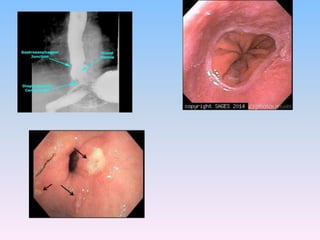
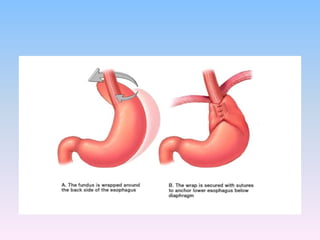
1) A hiatus hernia is a type of hernia where abdominal organs, usually the stomach, protrude into the chest cavity through the diaphragm.
2) Risk factors include obesity, old age, major trauma, and scoliosis. Hiatus hernias are caused by increased abdominal pressure from activities like lifting, coughing, vomiting, or straining.
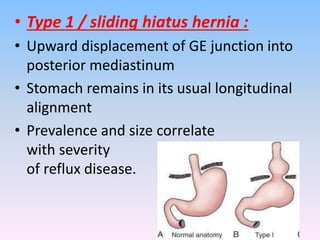
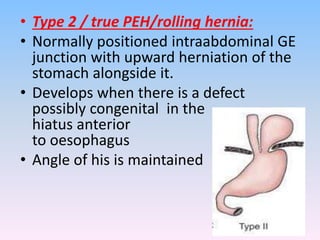
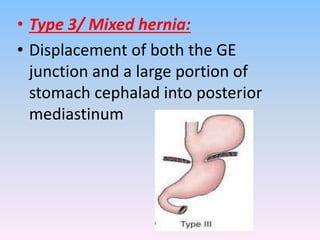
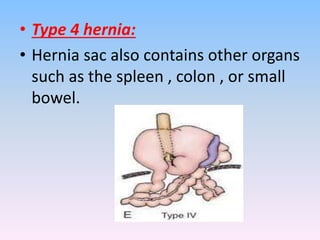
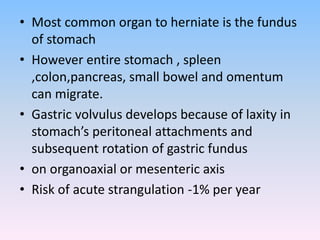
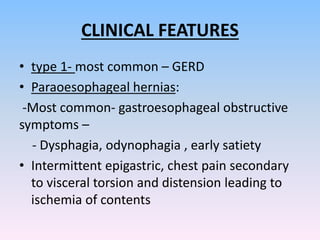
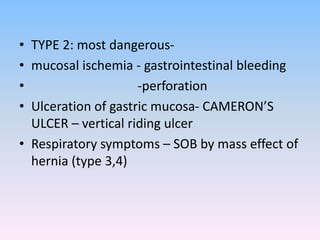
3) There are four types of hiatus hernia that vary based on which parts of the stomach protrude into the chest cavity. Type 1 is most common and involves reflux disease. Types 2 and 3 present a higher risk for complications like bleeding or perforation.