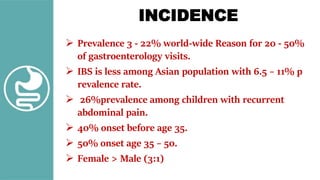
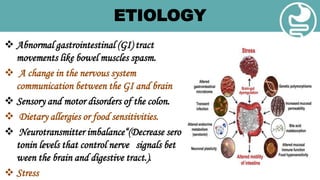
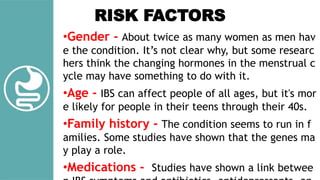
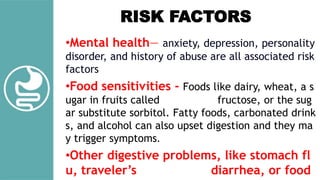
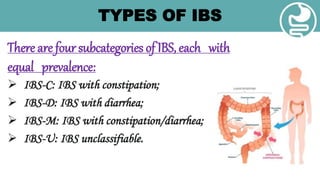
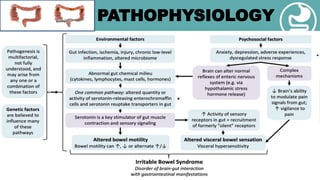
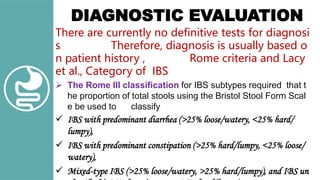
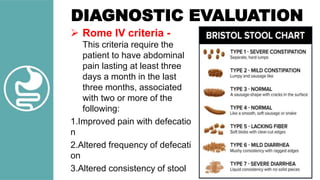
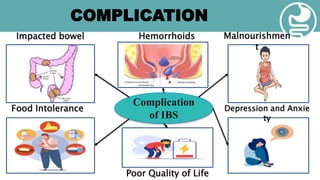
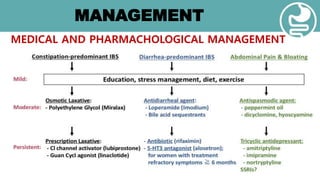
Irritable bowel syndrome (IBS) is a common functional disorder affecting the large intestine, characterized by recurrent abdominal pain and disordered bowel movements, prevalent in 3-22% of the population. Factors contributing to IBS include gastrointestinal tract irregularities, dietary sensitivities, mental health issues, and a familial tendency, with symptoms varying among individuals. Diagnosis is primarily based on patient history and symptoms, with management focusing on dietary changes, stress reduction techniques, and education on triggers.