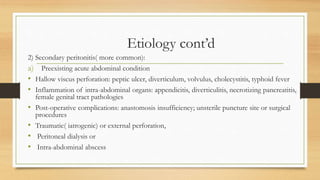
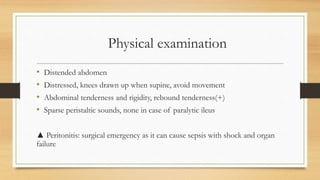
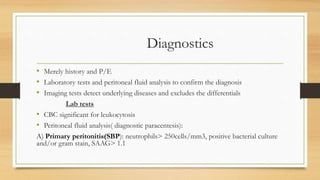
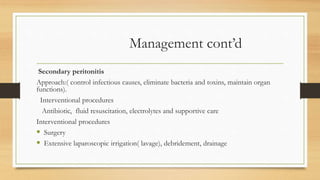
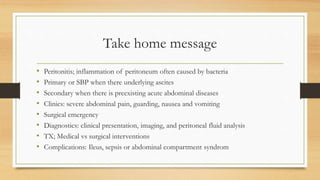
This document discusses peritonitis, which is inflammation of the peritoneum often caused by bacterial or fungal infections. It can be primary, secondary, or tertiary. Primary peritonitis occurs without an acute abdominal source, often in patients with ascites. Secondary peritonitis is more common and results from a preexisting acute abdominal condition like perforation or inflammation. Common causes, signs, diagnostic tests, treatment approaches, and complications are outlined. Management involves identifying and treating any infection through antibiotics and surgery as needed to control the infection, eliminate bacteria and toxins, and maintain organ function.