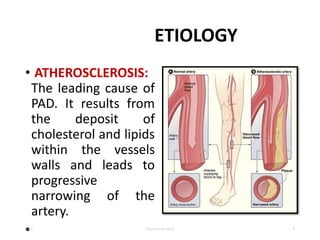
Peripheral artery disease (PAD) is a common circulatory problem where narrowed arteries reduce blood flow to the limbs, most commonly affecting the legs. It is usually caused by atherosclerosis and risk factors include smoking, diabetes, and hypertension. Symptoms may range from intermittent leg pain with walking to leg ulcers or gangrene. Diagnosis involves tests like ankle-brachial index and angiography. Treatment focuses on risk factor modification through medication, exercise and lifestyle changes, with surgical or minimally invasive procedures for more severe cases.