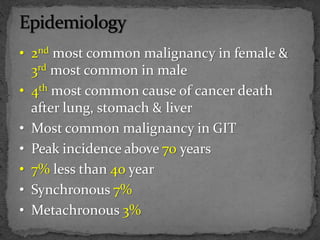
1. Colorectal cancer is the second most common malignancy in females and third most common in males. It is also the fourth most common cause of cancer death.
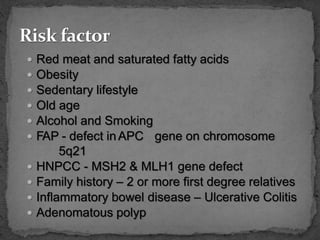
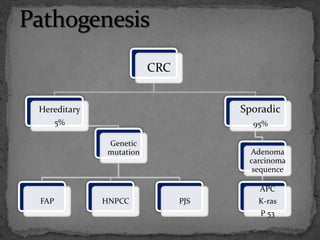
2. Risk factors include red meat, obesity, smoking, alcohol, family history, and inflammatory bowel disease. Most cases are sporadic but some are hereditary.
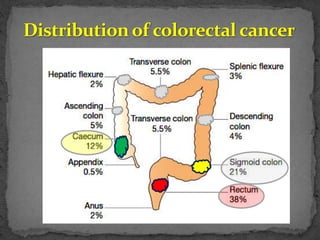
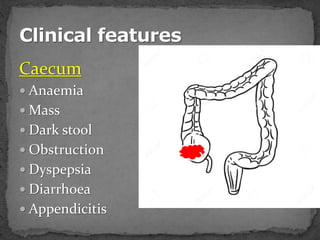
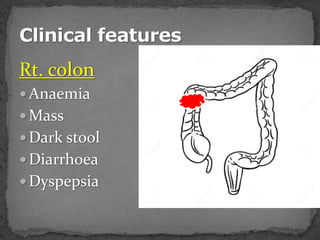
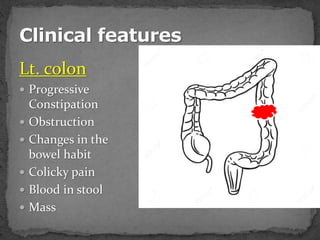
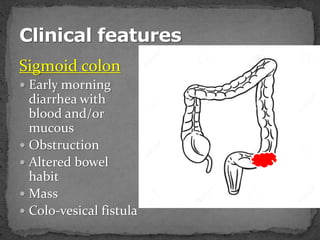
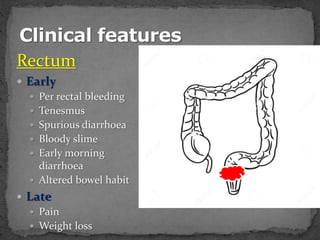
3. Symptoms depend on the location of the cancer in the colon but may include blood in stool, changes in bowel habits, abdominal pain, weight loss, and anemia.
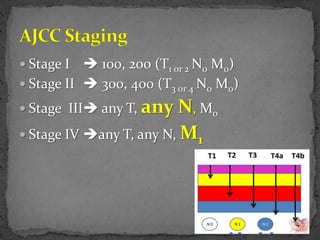
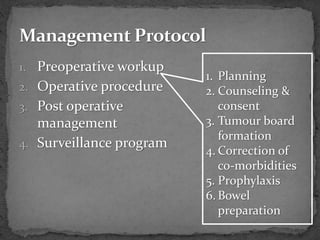
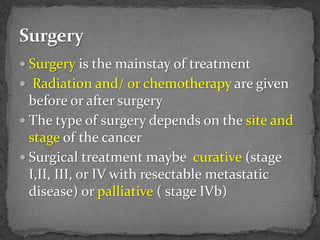
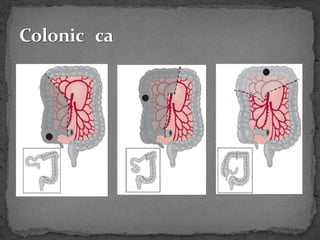
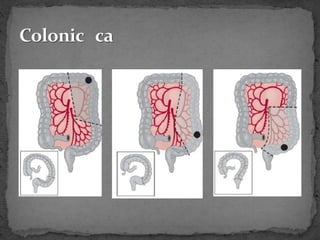
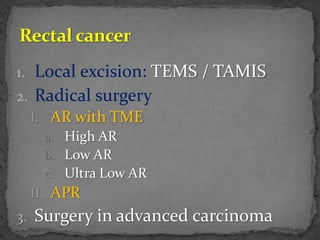
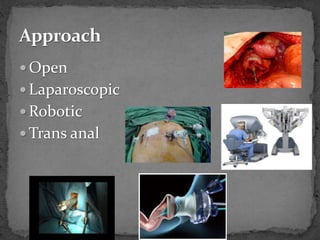
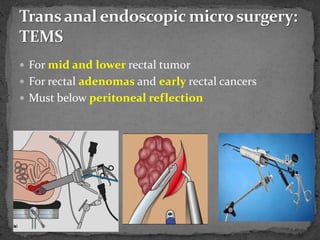
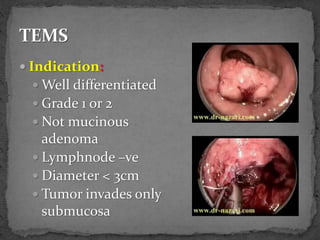
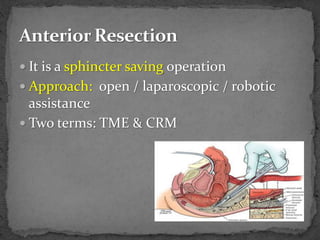
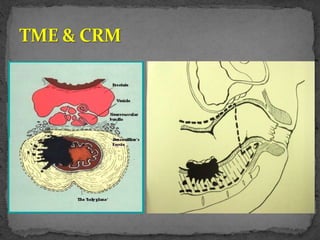
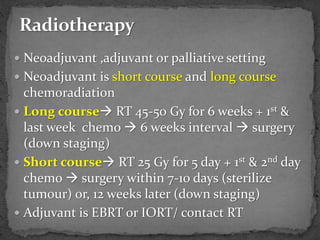
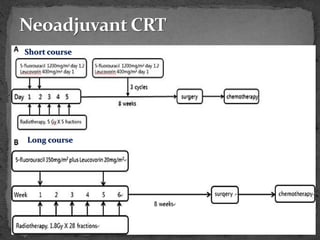
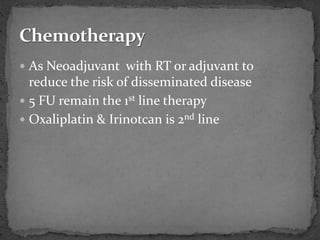
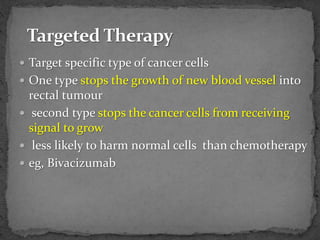
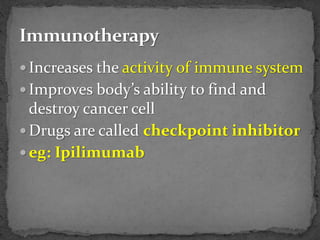
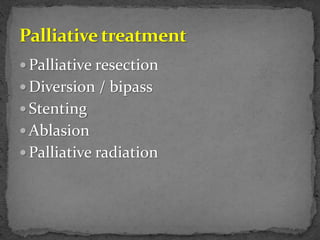
4. Treatment involves surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy depending on the stage and characteristics of the cancer. The type of surgery performed also depends on the location and