Peripheral arterial disease (PAD) is the obstruction or deterioration of arteries other than those supplying the heart and brain. PAD prevalence increases with age and is more common in Black individuals compared to Whites. A study in Ghana found higher PAD prevalence in Ghanaians living in Ghana compared to migrant Ghanaians in Europe. Risk factors for PAD include smoking, hypertension, diabetes, hyperlipidemia, and renal insufficiency. Treatment involves lifestyle modifications, medications, and revascularization procedures like angioplasty, stenting, or bypass surgery depending on the severity and location of arterial blockages. Amputations may be required for gangrenous or critically ischemic limbs.



![PAD in GHANA
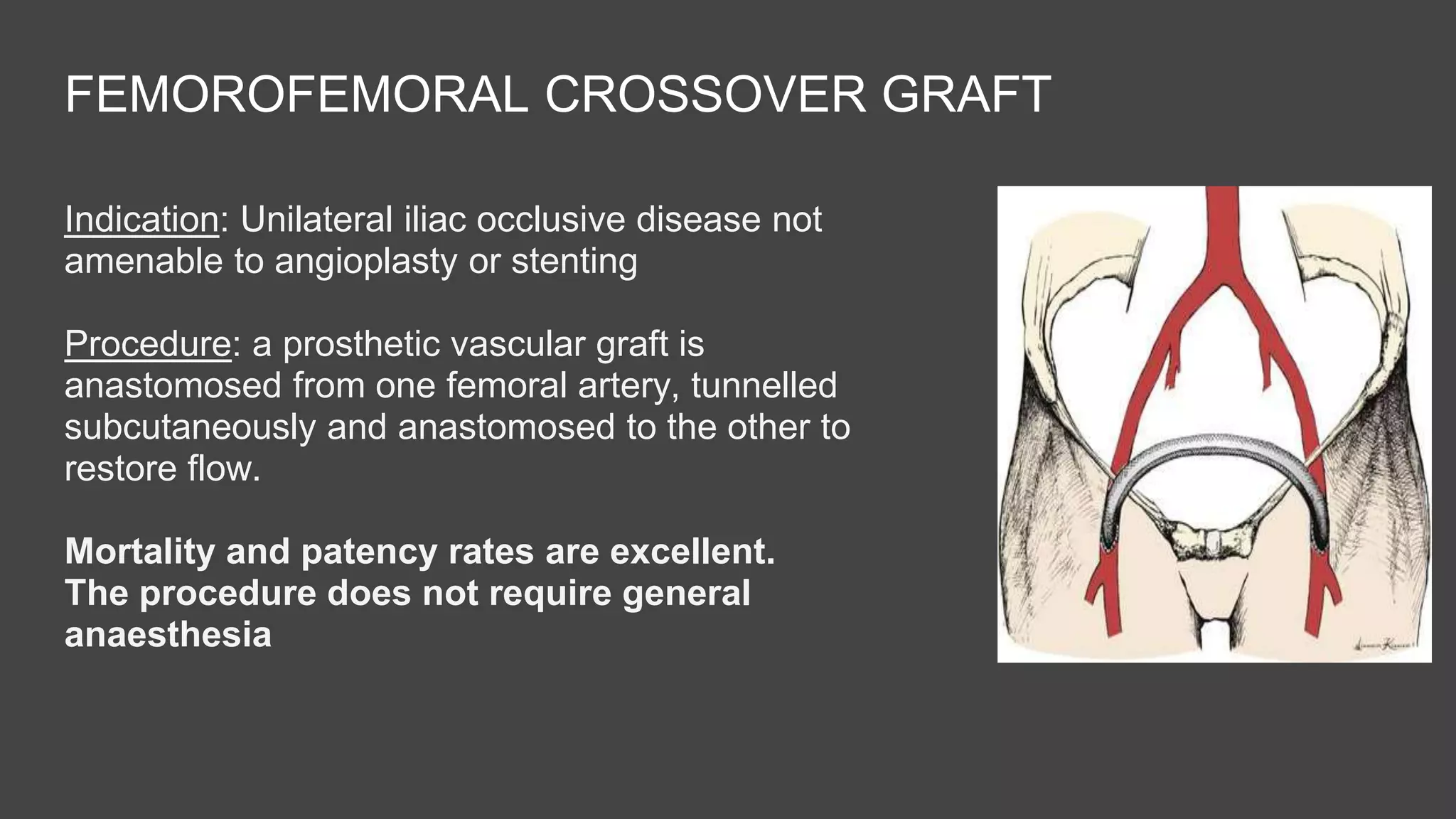
n=5516
Europe - (1487 Amsterdam, 546 Berlin,
1047 London) and Ghana [1419 urban
and 1017 rural] aged 25–70 yrs
Conc: Ghanaians living in Ghana have
higher prevalence of PAD than their
migrant compatriots
Case-control n=623 Anthropometric indices assessed
PAD (ABI ≤ 0.9, n = 261) and non-PAD (ABI > 0.9, n = 362) groups
PAD participants had higher BMI and waist
circumference than non-PAD participants
PAD participants had higher BMI and waist
circumferences than non-PAD participants
BMI ≥ 30 kg/m2 was associated with twofold increase in the odds of PAD.](https://image.slidesharecdn.com/peripheralarterialdisease-210325223200/75/Peripheral-Arterial-Disease-4-2048.jpg)