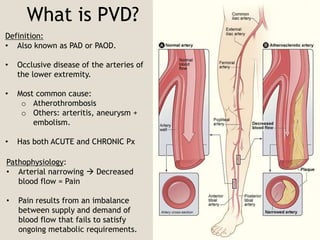
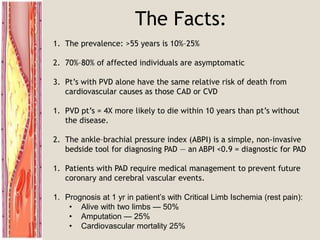
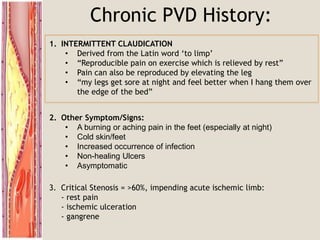
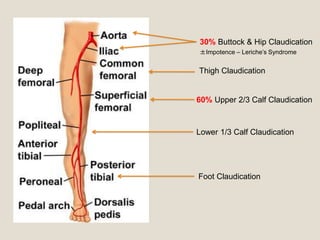
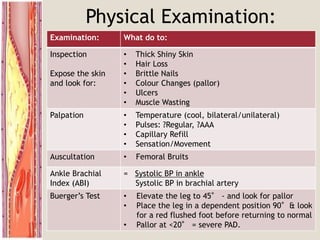
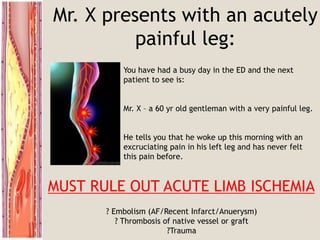
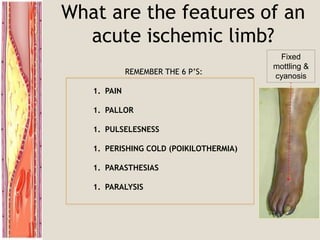
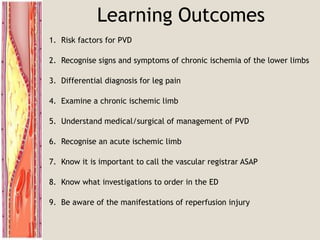
Peripheral vascular disease (PVD), also known as peripheral artery disease (PAD), is a common cause of limb ischemia characterized by atherosclerotic narrowing of the arteries in the lower extremities. It can present acutely with critical limb ischemia manifested as severe pain, pallor, pulselessness, coldness and potential paralysis, or chronically with intermittent claudication pain on exertion that resolves with rest. PVD risk factors include smoking, diabetes, hypertension, hyperlipidemia and age over 70. Treatment involves risk factor modification, exercise rehabilitation, medical management with antiplatelets and cilostazol, as well as endovascular or surgical revascularization for severe symptoms or limb threatening ischemia. Acute