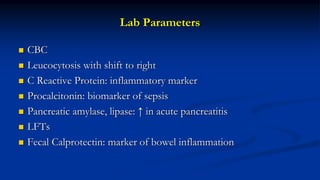
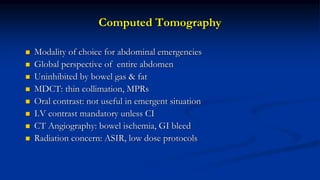
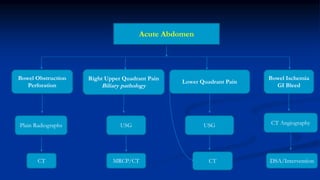
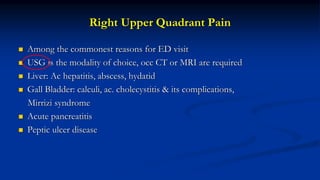
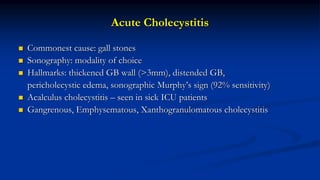
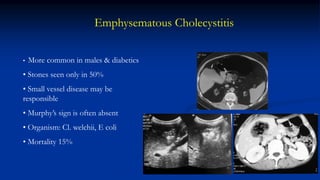
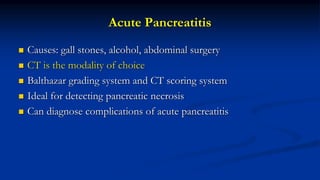
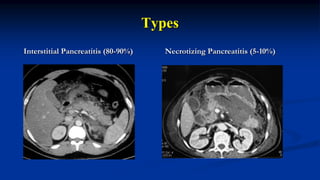
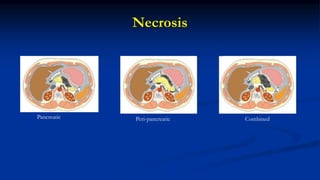
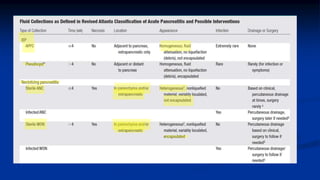
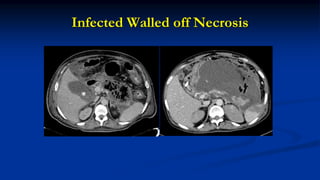
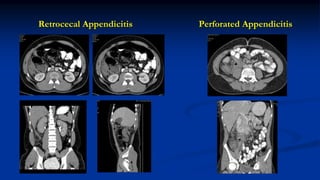
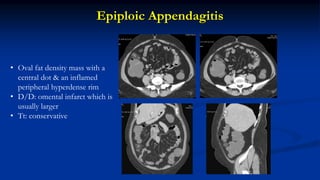
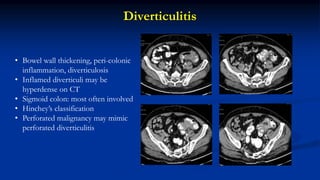
Clinical and imaging inputs are important for diagnosing acute abdominal inflammatory conditions. A thorough history and physical exam can provide clues to the condition. Key lab tests include a CBC, CRP, and pancreatic enzymes. Imaging plays a crucial role, with ultrasound as a first-line exam and CT being the preferred modality. CT allows evaluation of the entire abdomen and detection of complications. The clinical presentation and location of pain can help determine the appropriate imaging exam and differential diagnoses to consider.