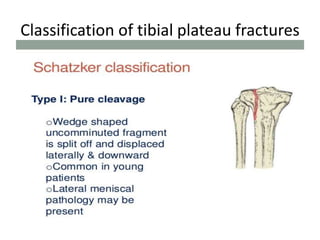
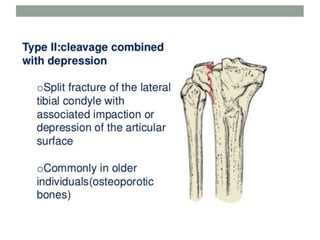
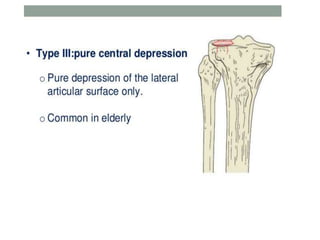
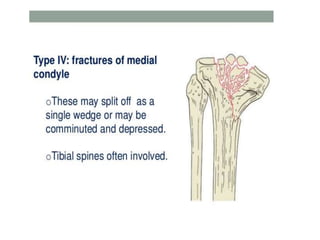
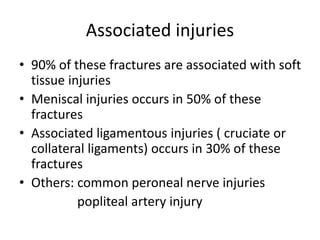
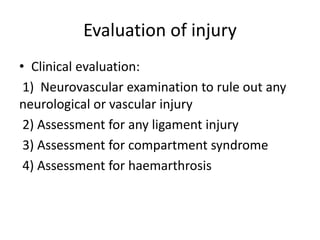
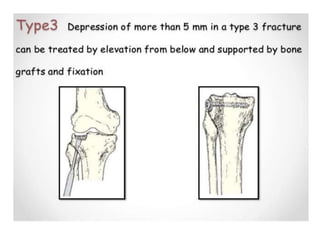
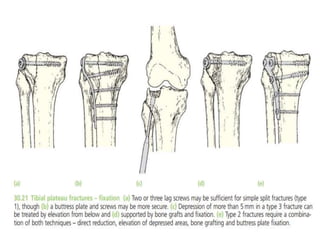
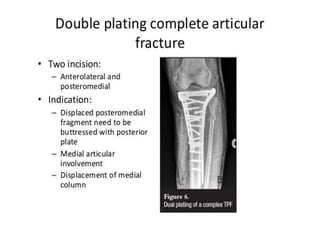
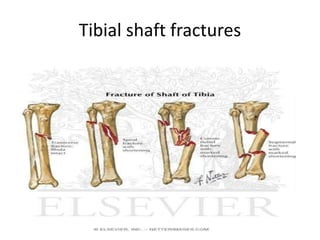
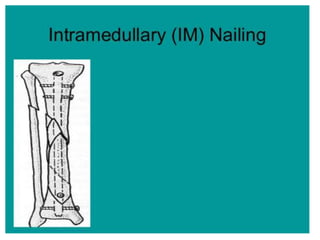
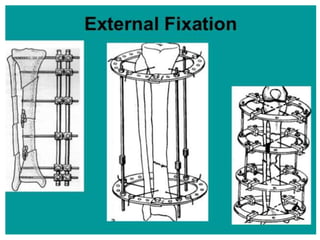
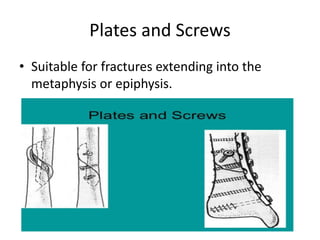
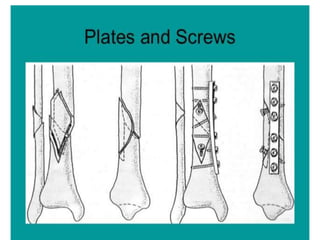
Tibial fractures can occur in the tibial plateau or tibial shaft. Tibial plateau fractures comprise 1% of all fractures and are usually caused by high-energy injuries involving axial loading and valgus/varus forces on the knee. They are often associated with soft tissue injuries. Tibial shaft fractures are commonly caused by direct trauma from motor vehicle accidents and may be open or closed fractures. Treatment depends on the fracture type but commonly involves internal fixation methods like intramedullary nailing or plating. Complications can include malunion, delayed healing, and infections.