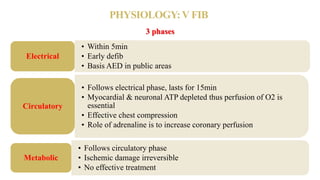
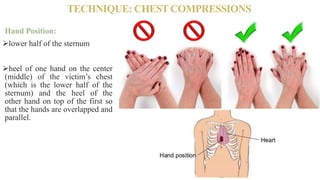
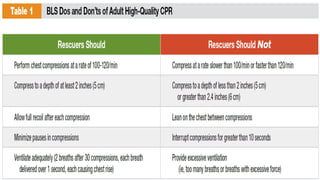
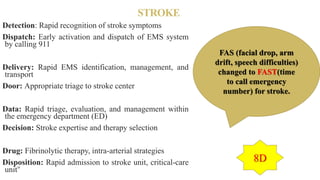
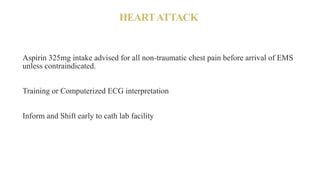
This document summarizes a multidisciplinary conference on basic life support presented by Dr. Ravikiran H M. It defines BLS and describes the key techniques including chest compressions, ventilation, use of an AED, and management of foreign body airway obstruction. The physiology of cardiac arrest and importance of early defibrillation are explained. When and when not to start CPR, potential harms, special situations like opioid overdose and stroke, and references are also summarized. The document provides an overview of best practices in basic life support.