The document provides information on pediatric resuscitation. It discusses:
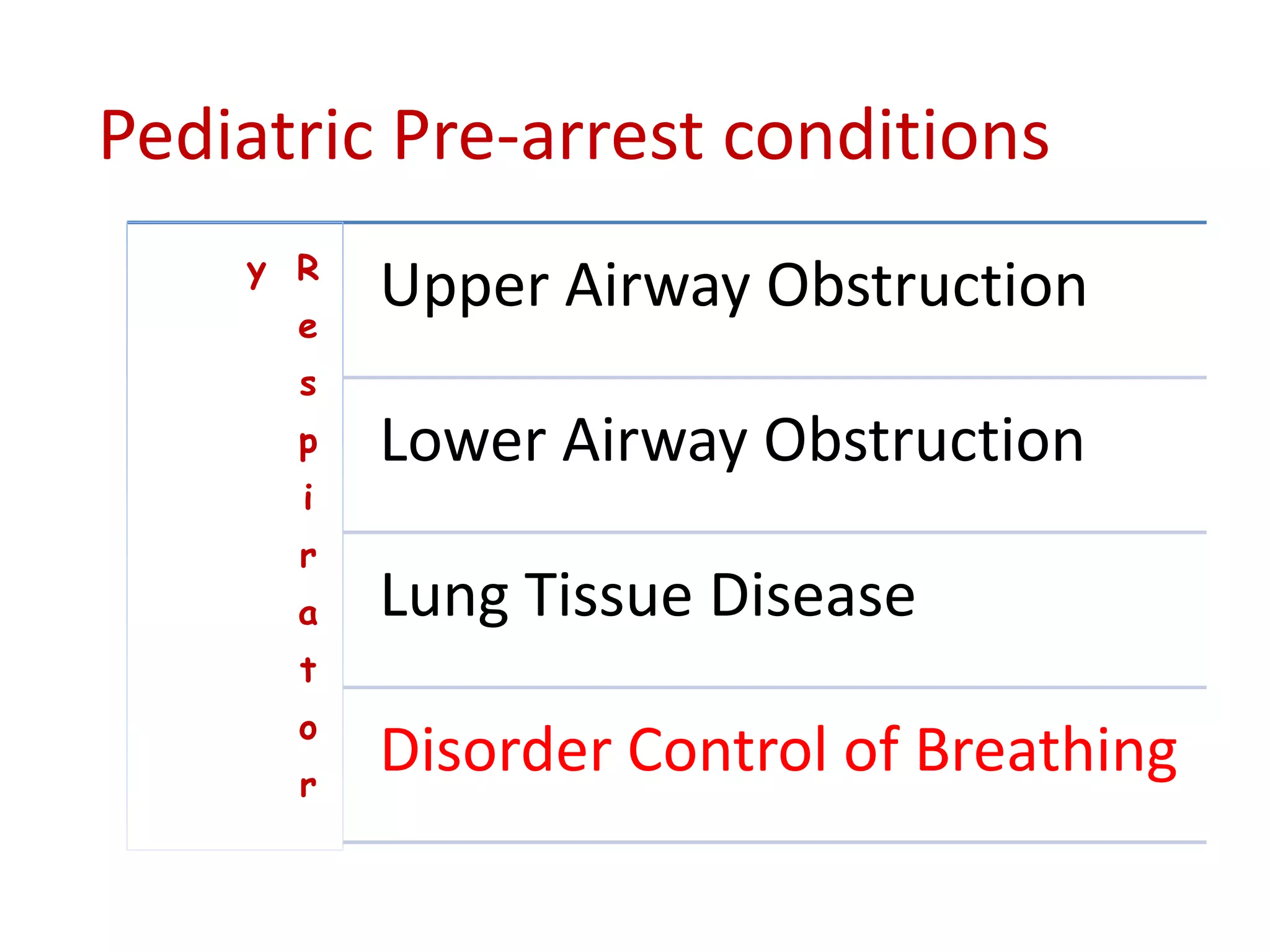
1) Poor survival rates of 4-13% for out-of-hospital pediatric cardiac arrest, though in-hospital is higher at 27%. Early prevention through recognition of respiratory distress or shock can improve outcomes.
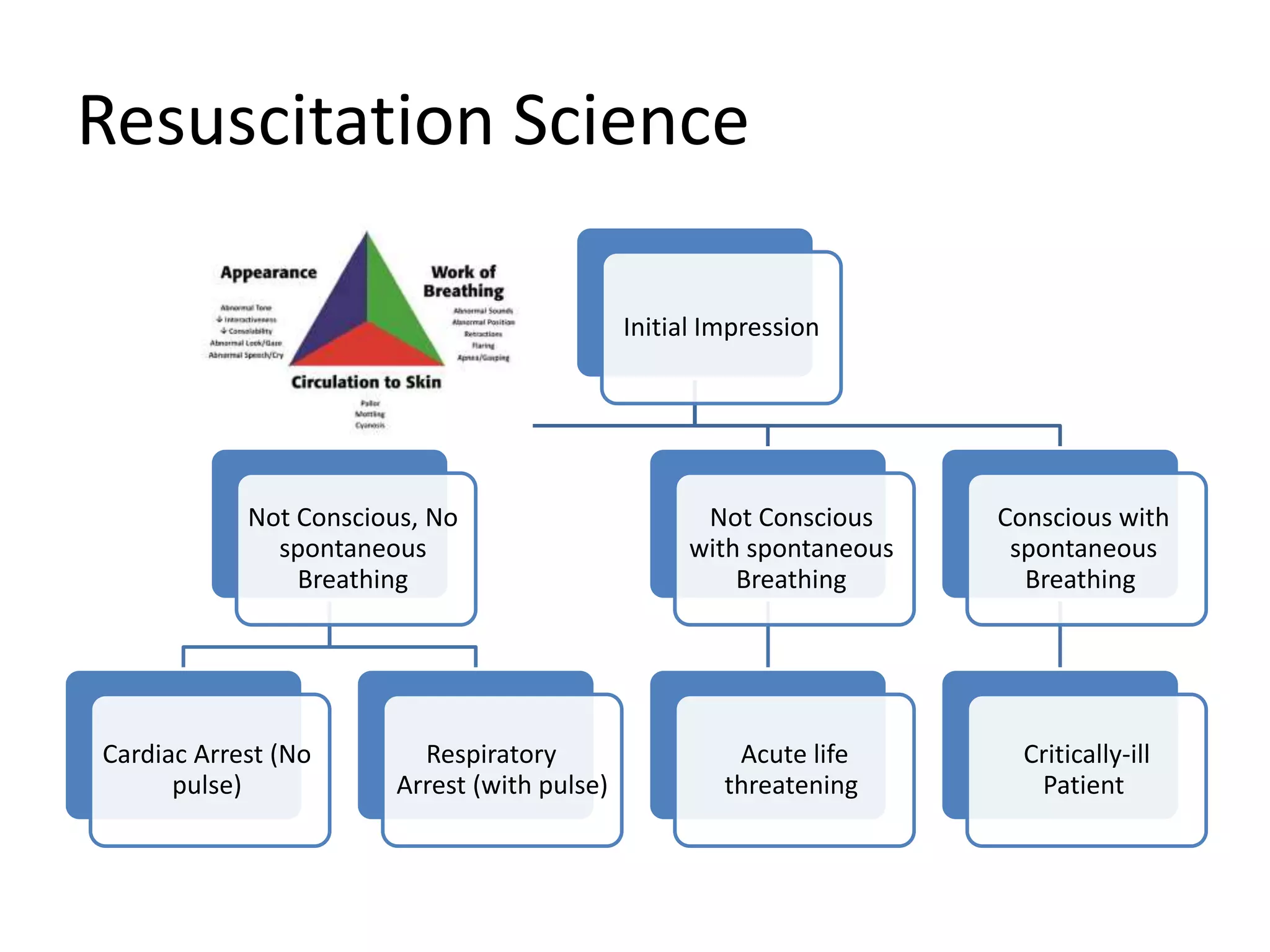
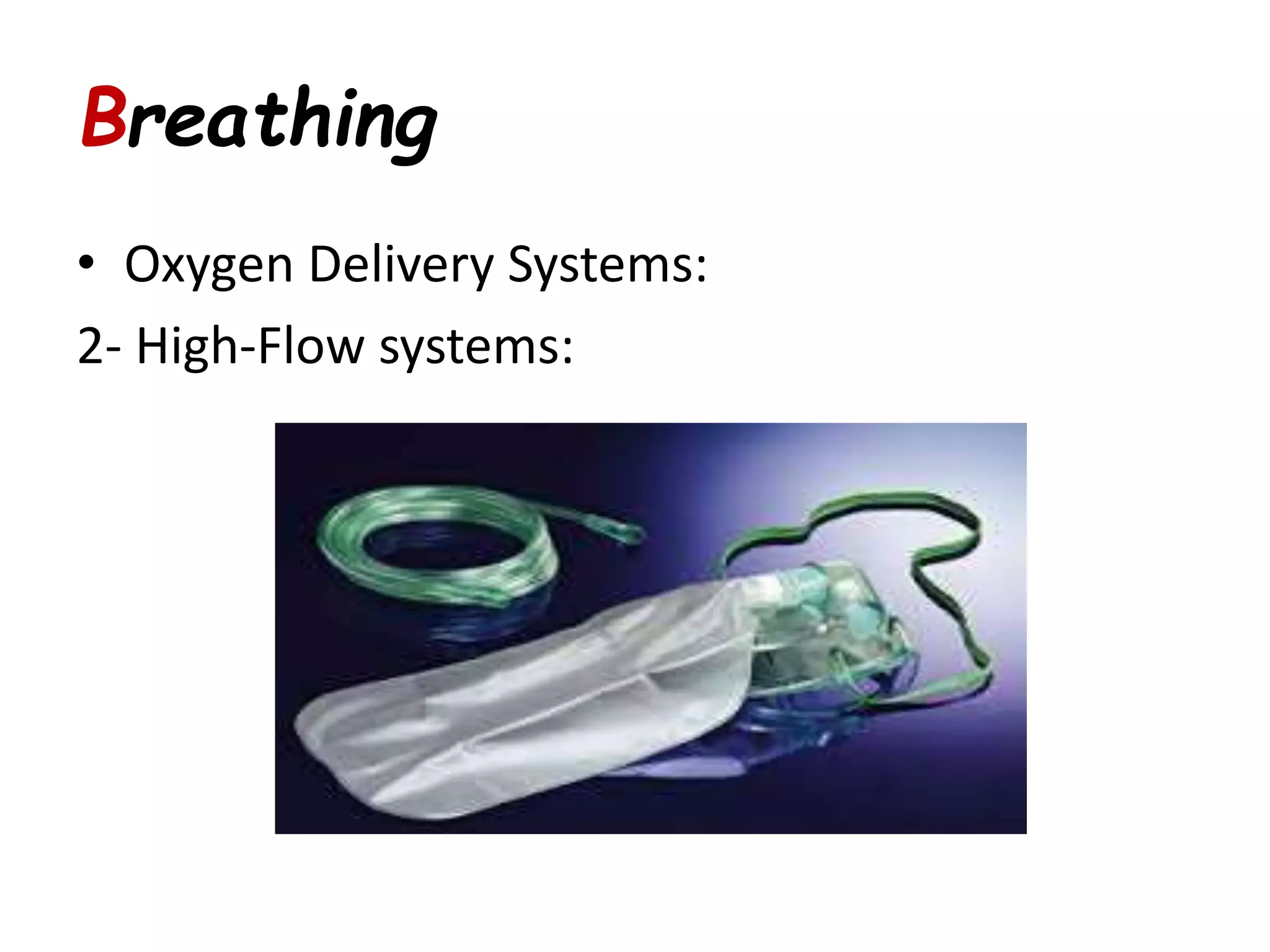
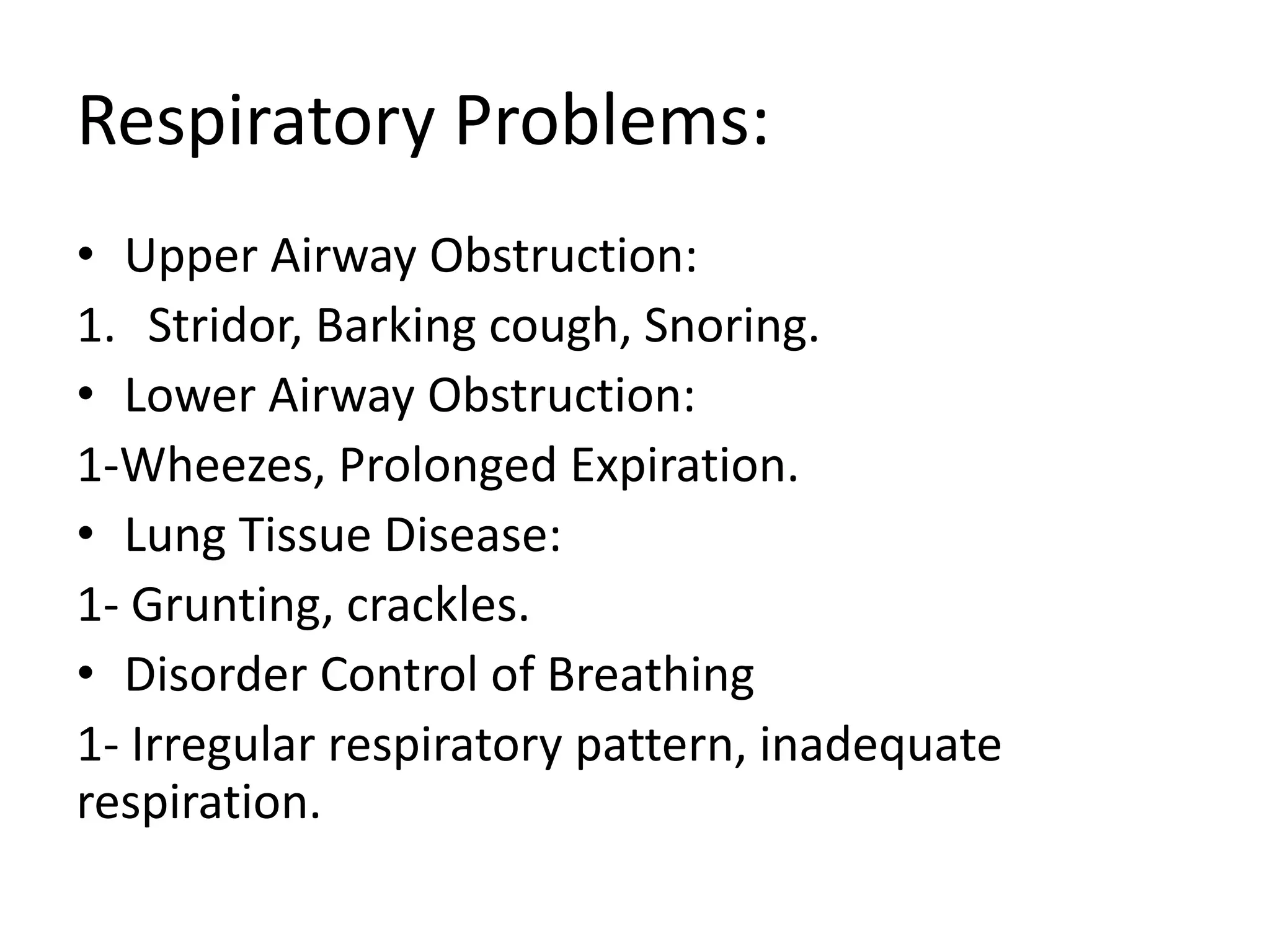
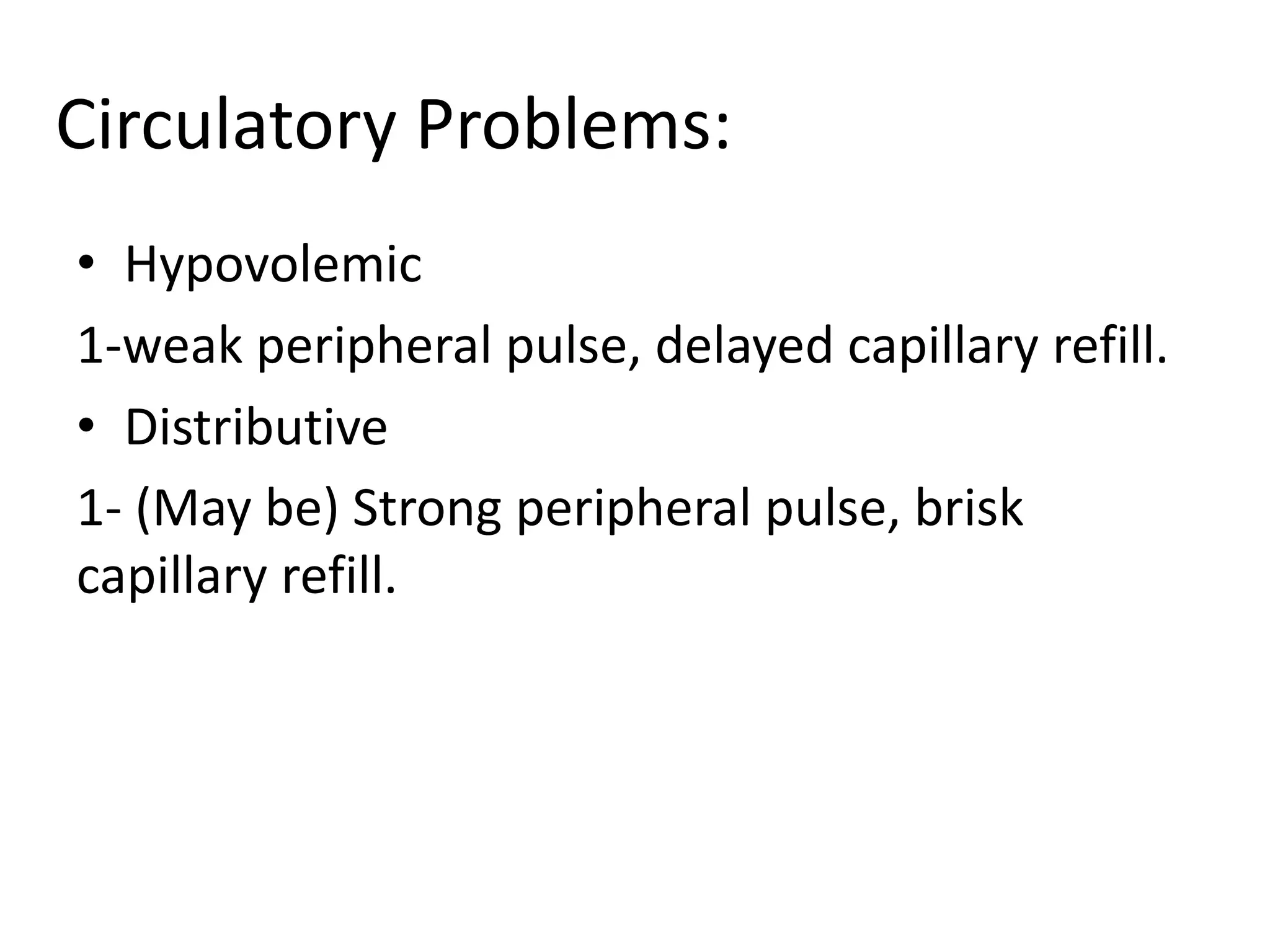
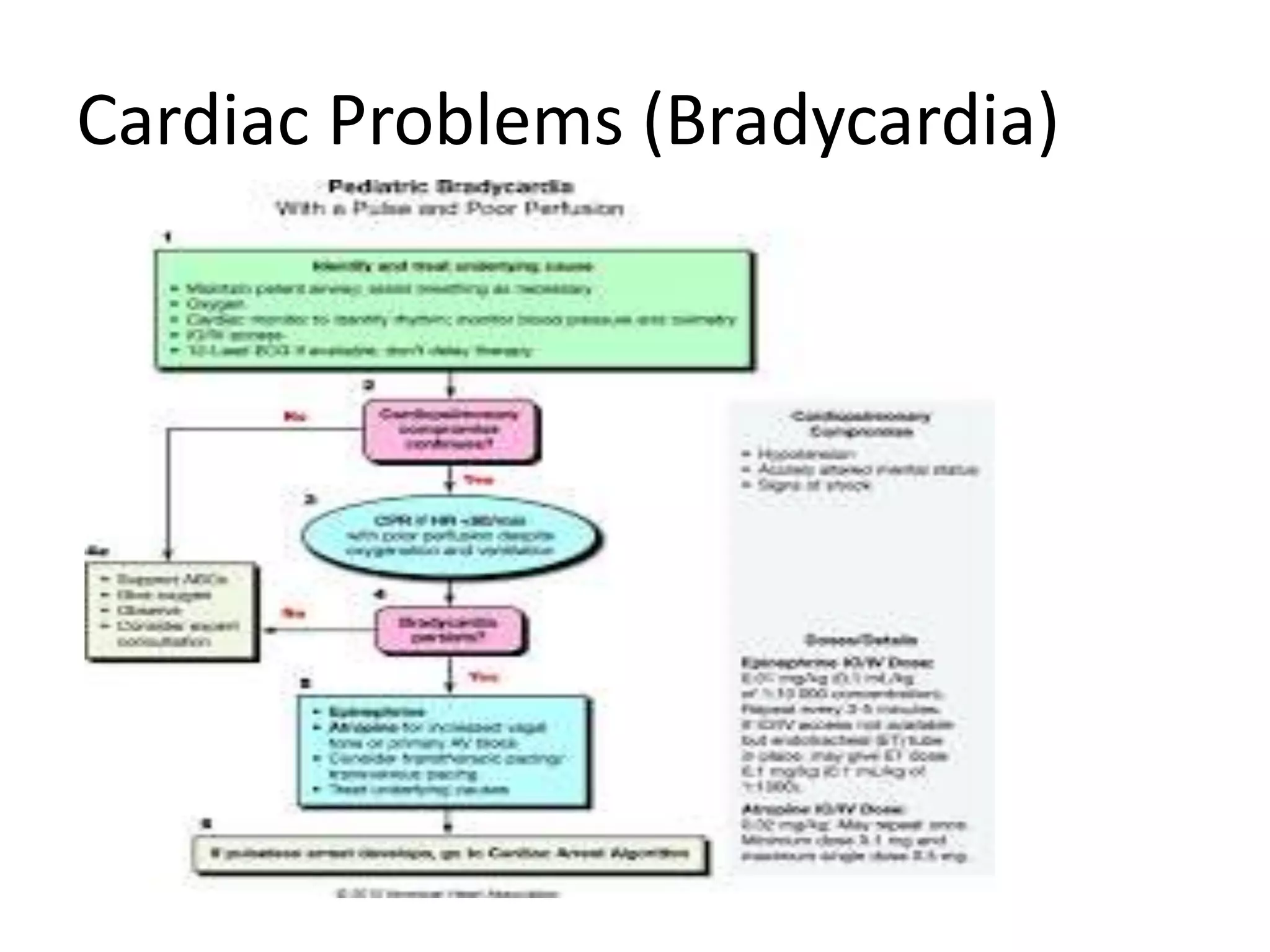
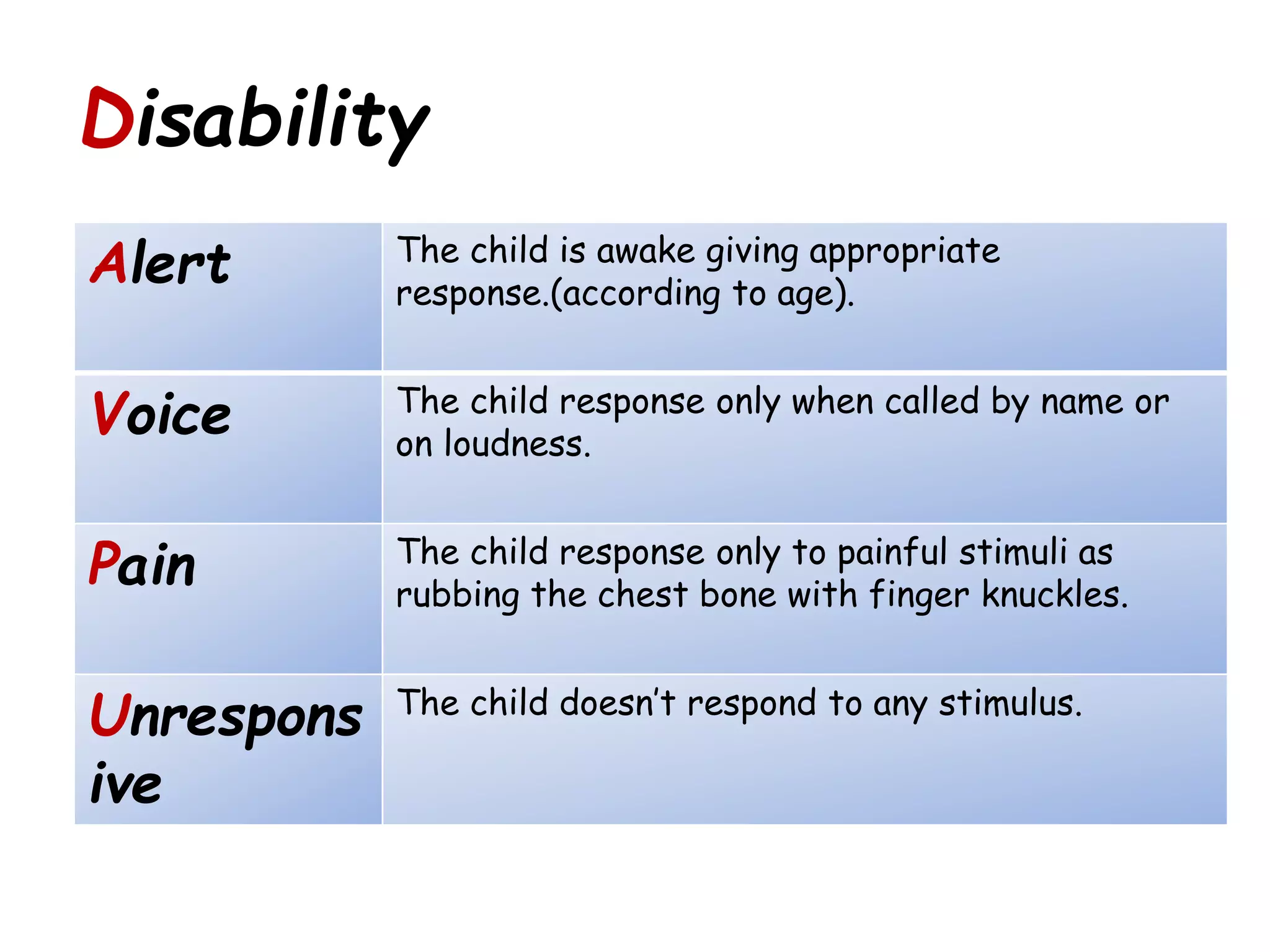
2) A systematic approach following the pediatric chain of survival - assessing airway, breathing, circulation, disability, and exposure.
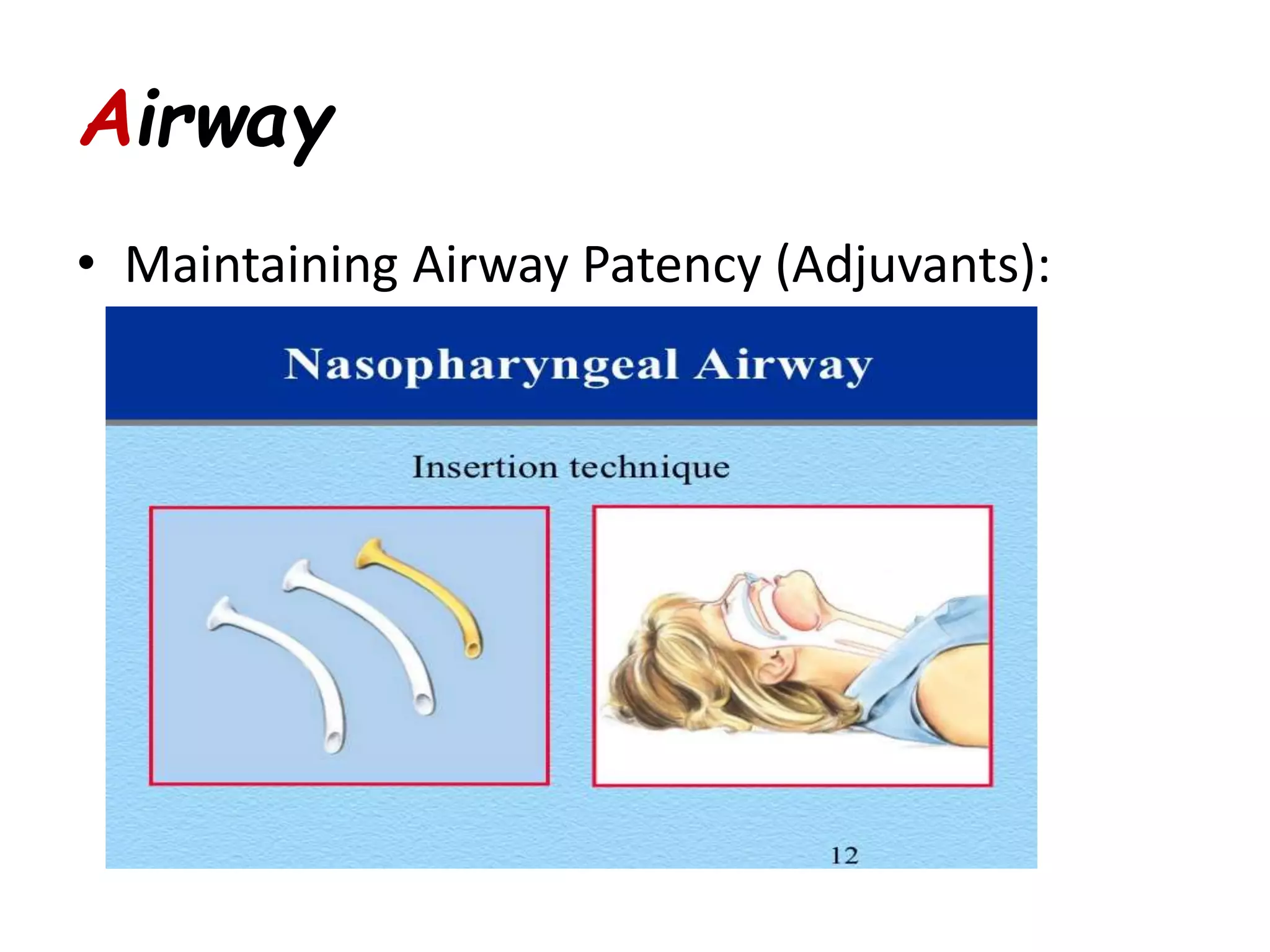
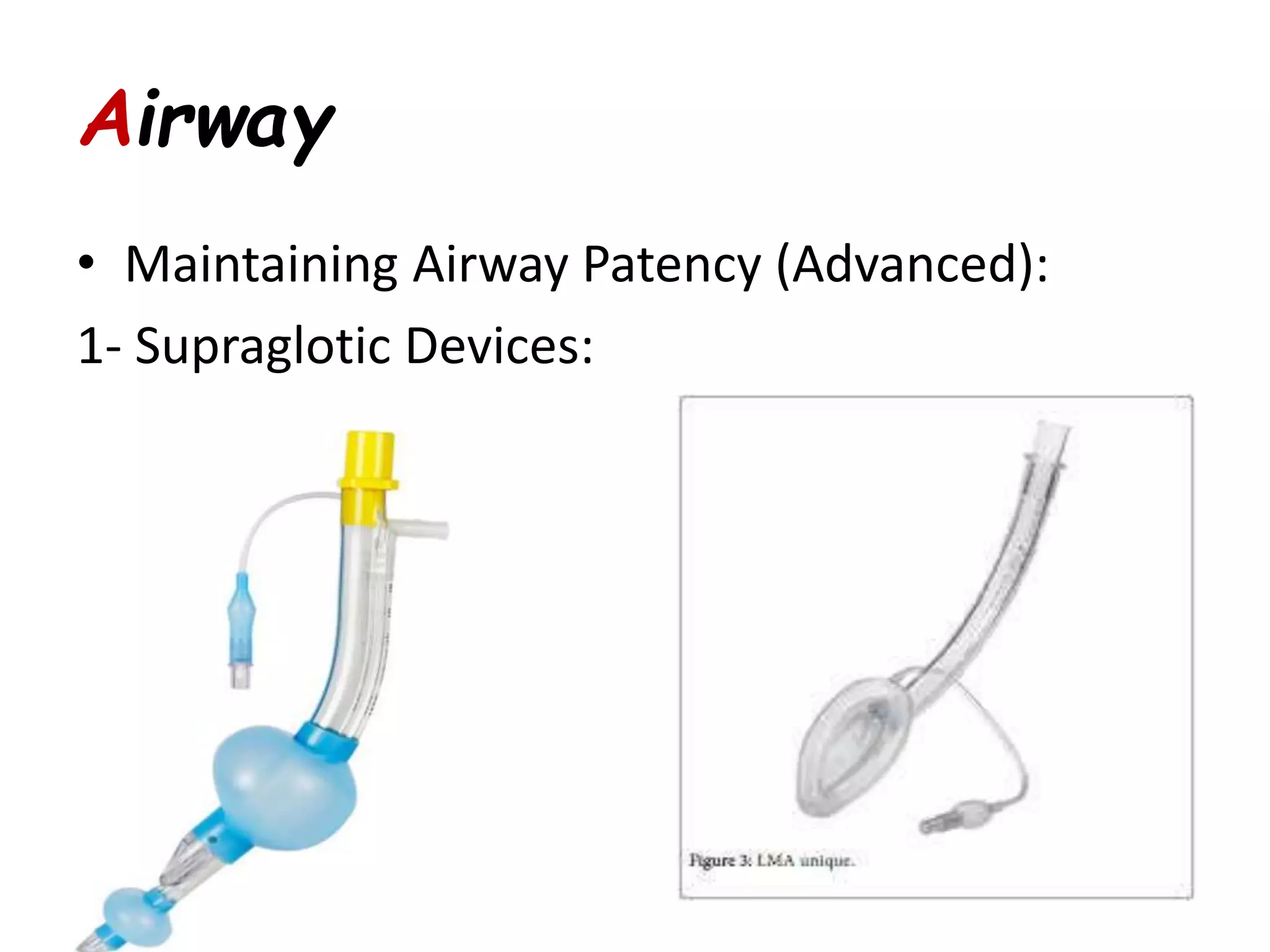
3) Key differences in pediatric resuscitation including airway anatomy and techniques for opening and maintaining the airway. Emphasis is placed on high-quality chest compressions and minimizing interruptions during CPR.