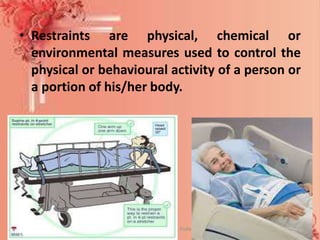
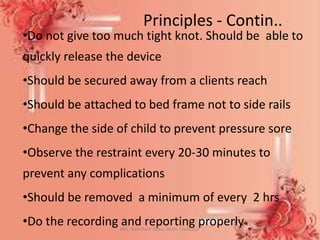
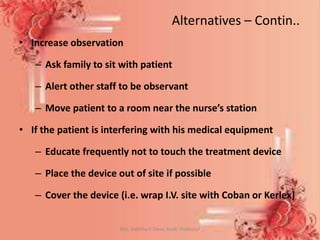
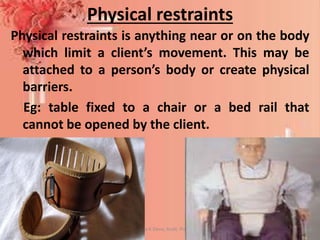
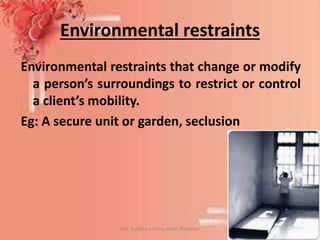
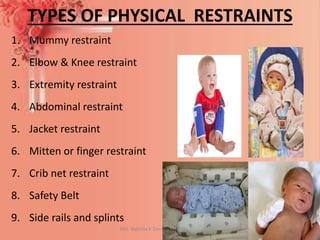
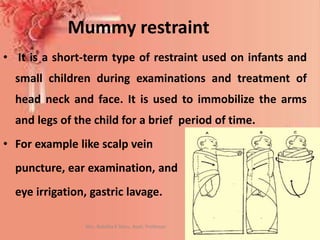
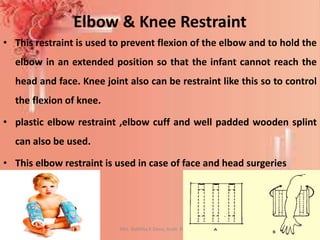
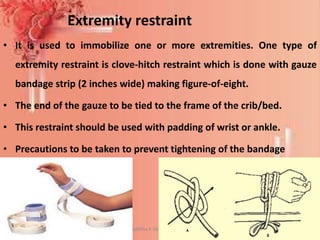
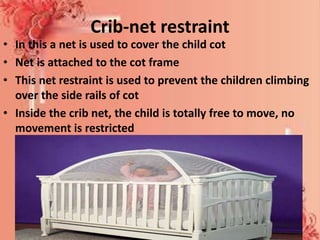
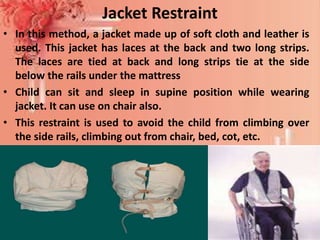
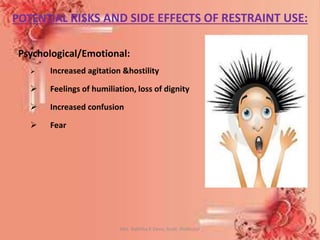
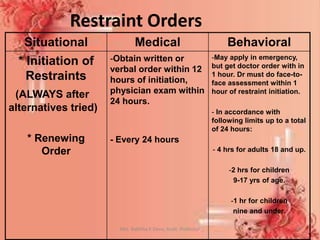
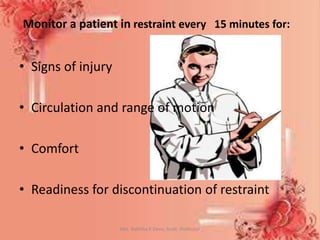
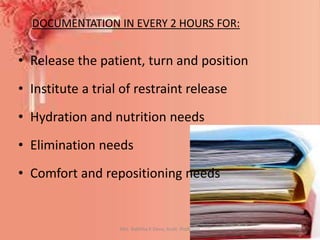
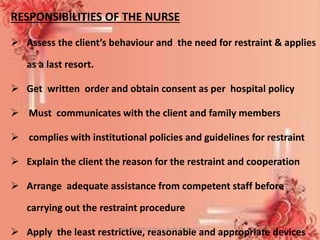
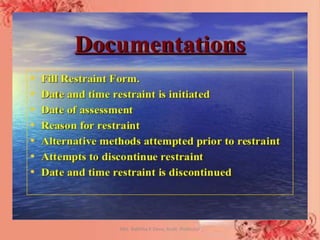
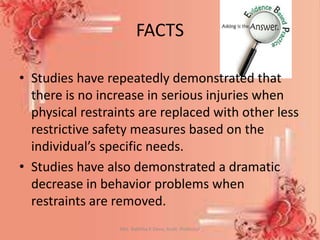
The document discusses child restraints, including definitions, purposes, types, risks, and the nurse's role. It defines restraint as the intentional restriction of movement and describes physical, chemical, and environmental restraints. Common physical restraints for children include mummy restraints, elbow/knee restraints, extremity restraints, abdominal restraints, mittens, crib nets, and jackets. Risks of restraint use include psychological, physical, and in some cases death. Nurses must monitor restrained patients closely, document regularly, and follow policies and guidelines for safe and appropriate restraint.