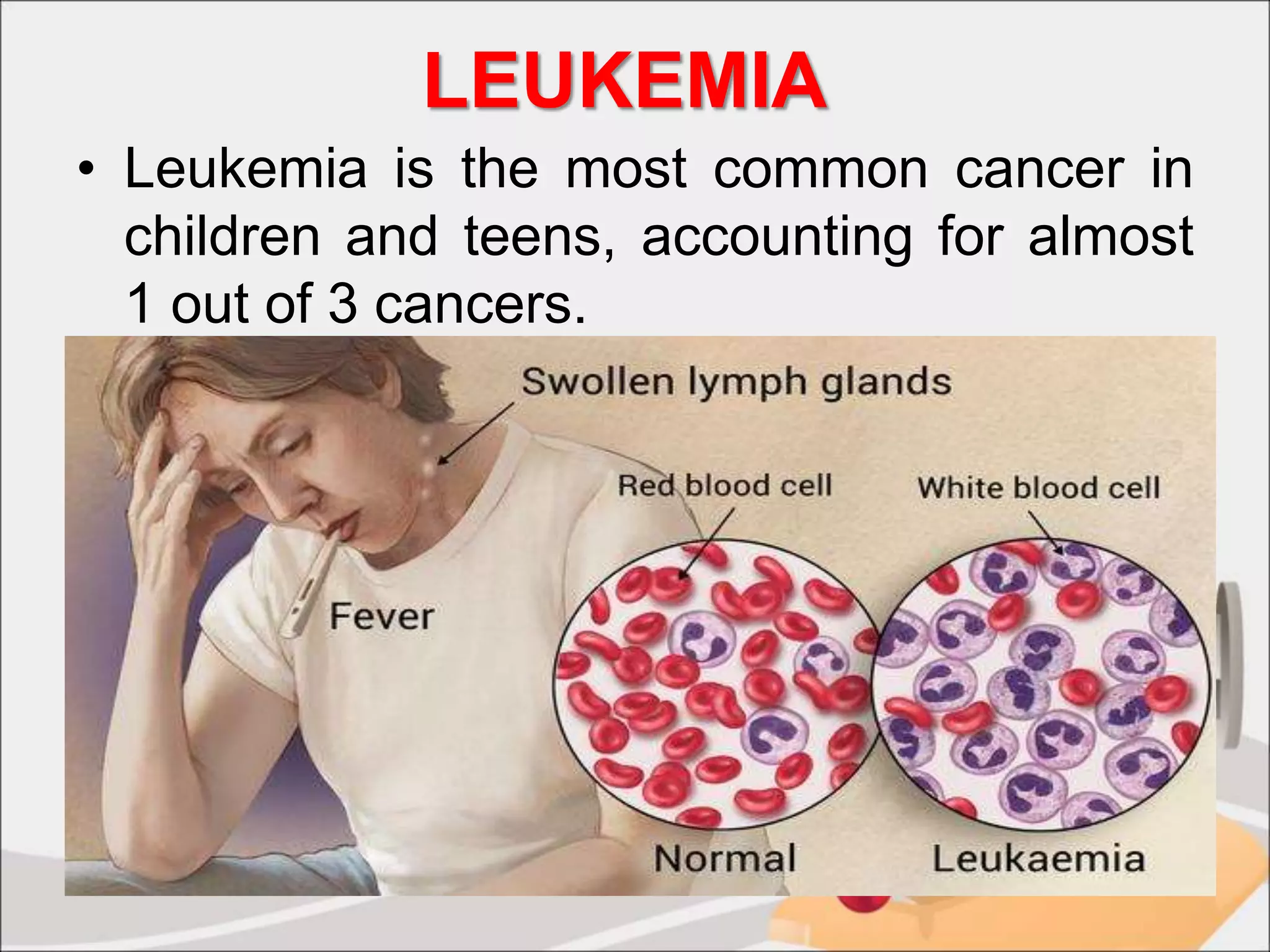
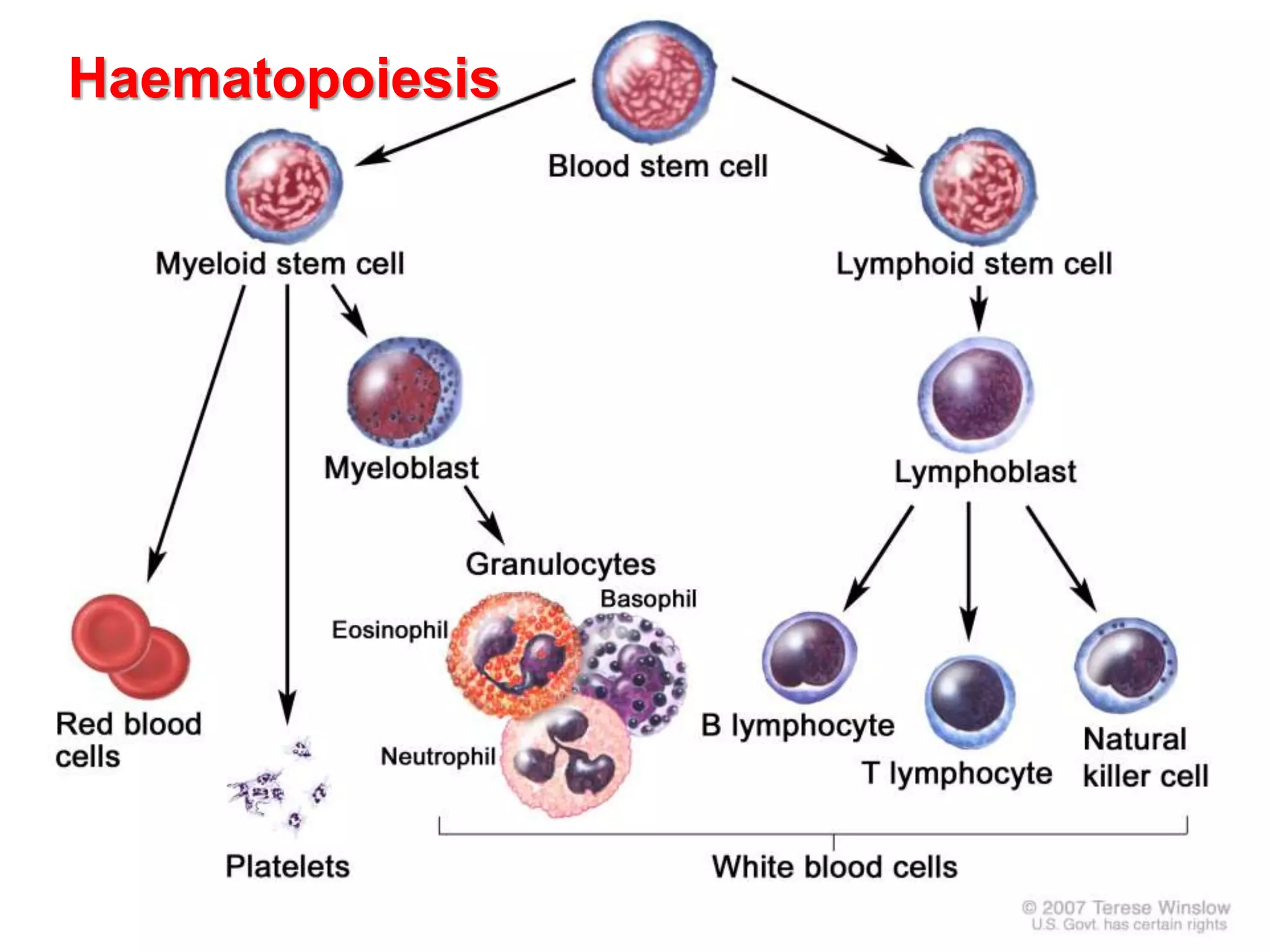
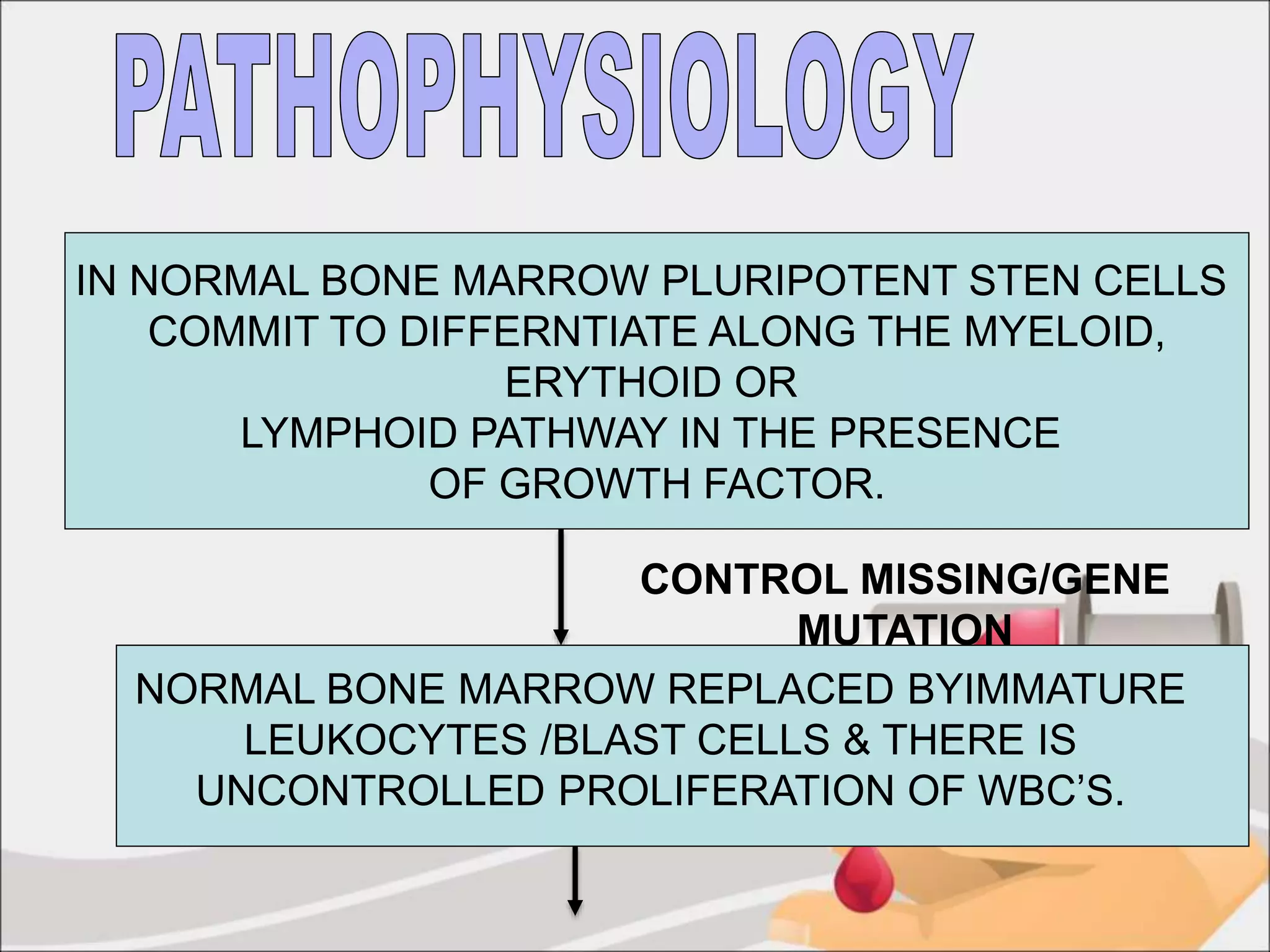
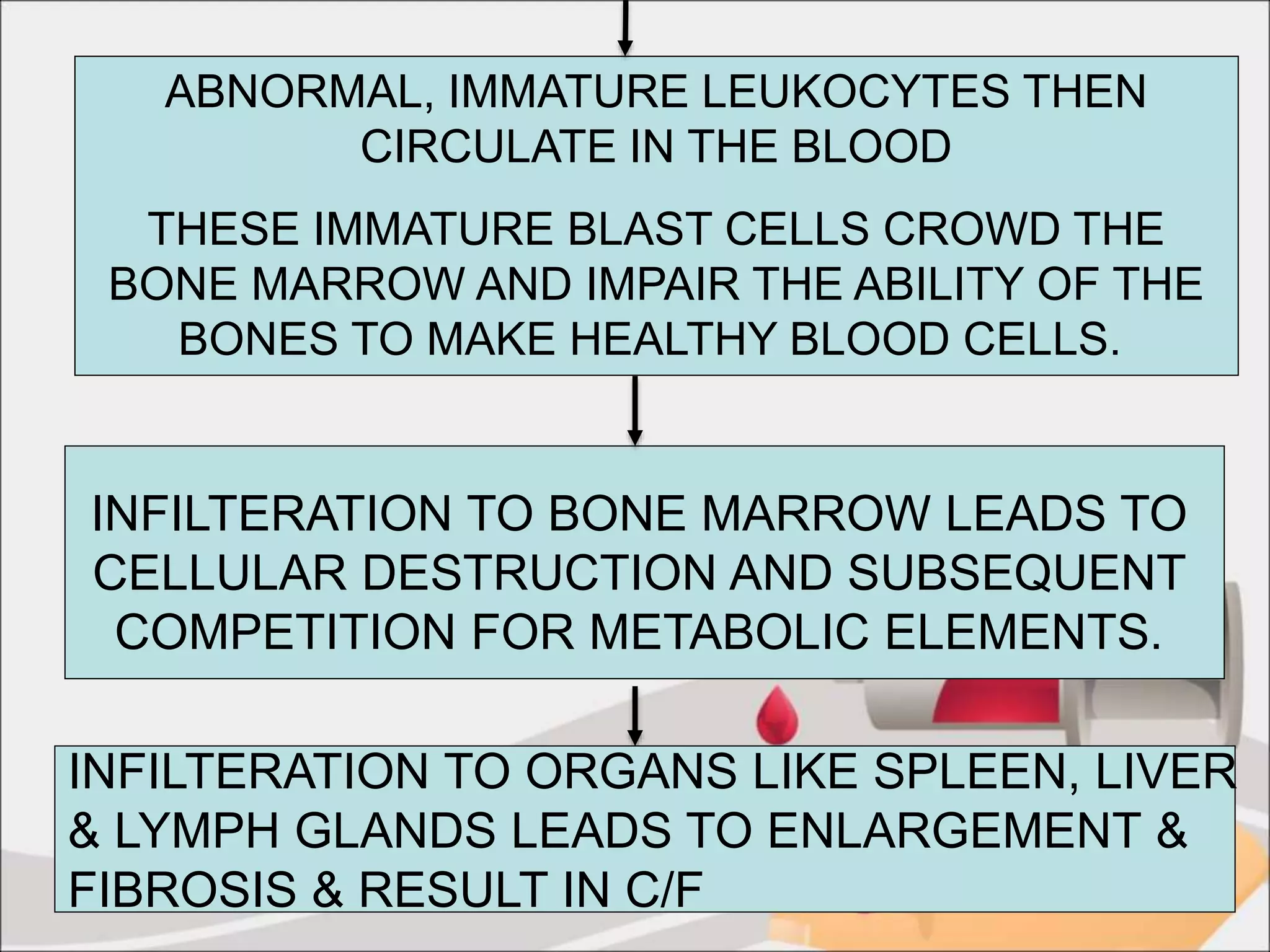
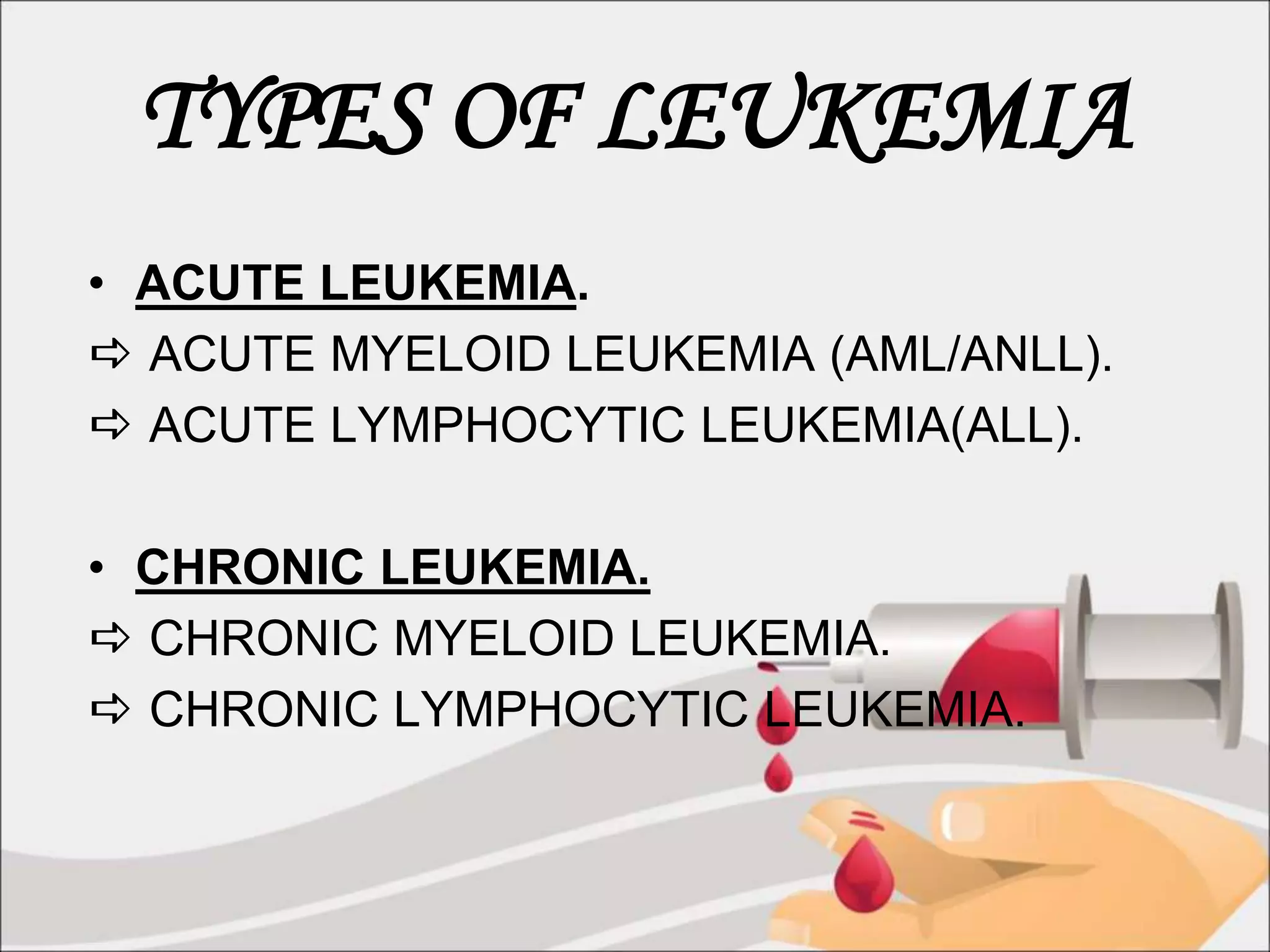
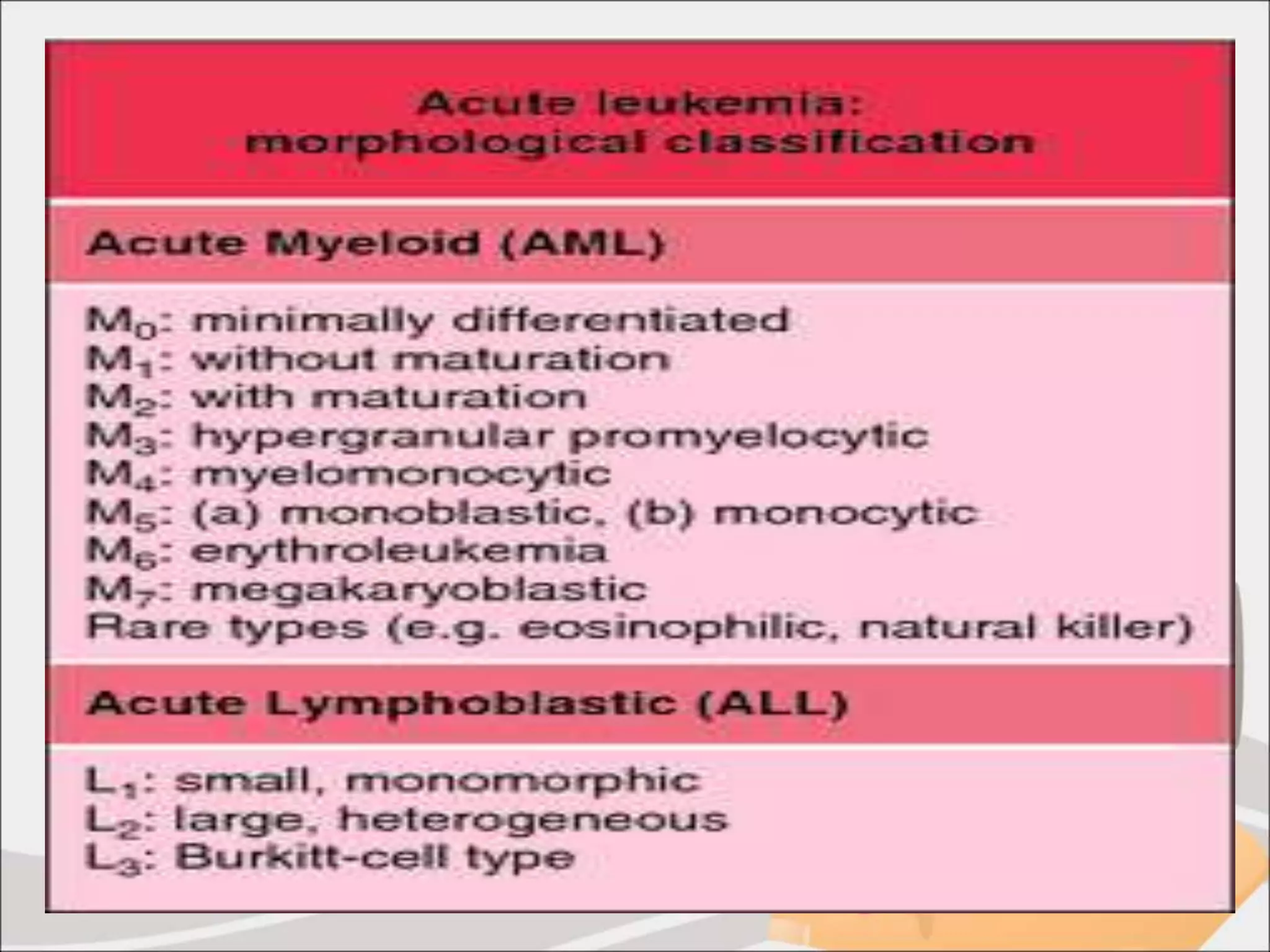
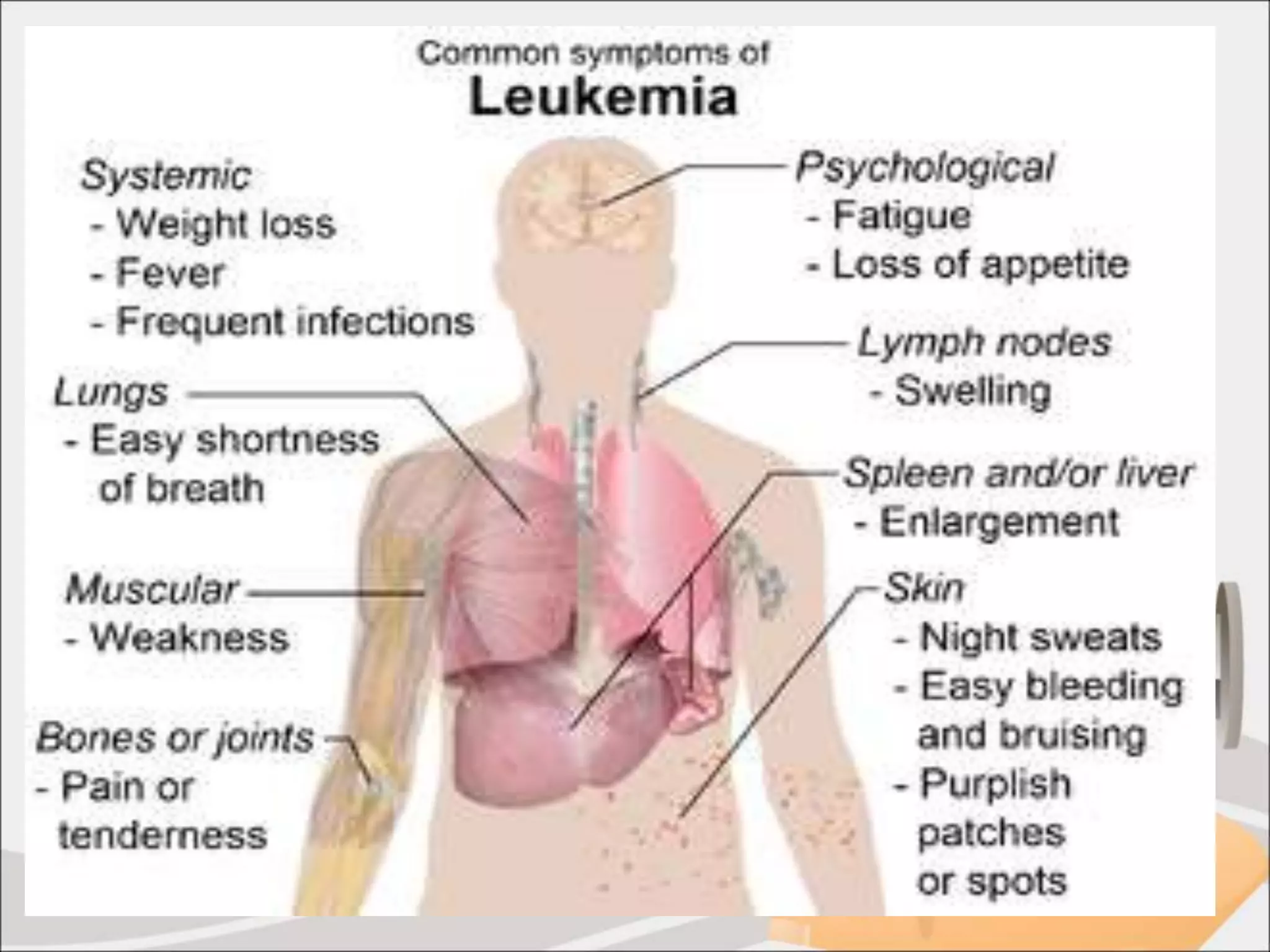
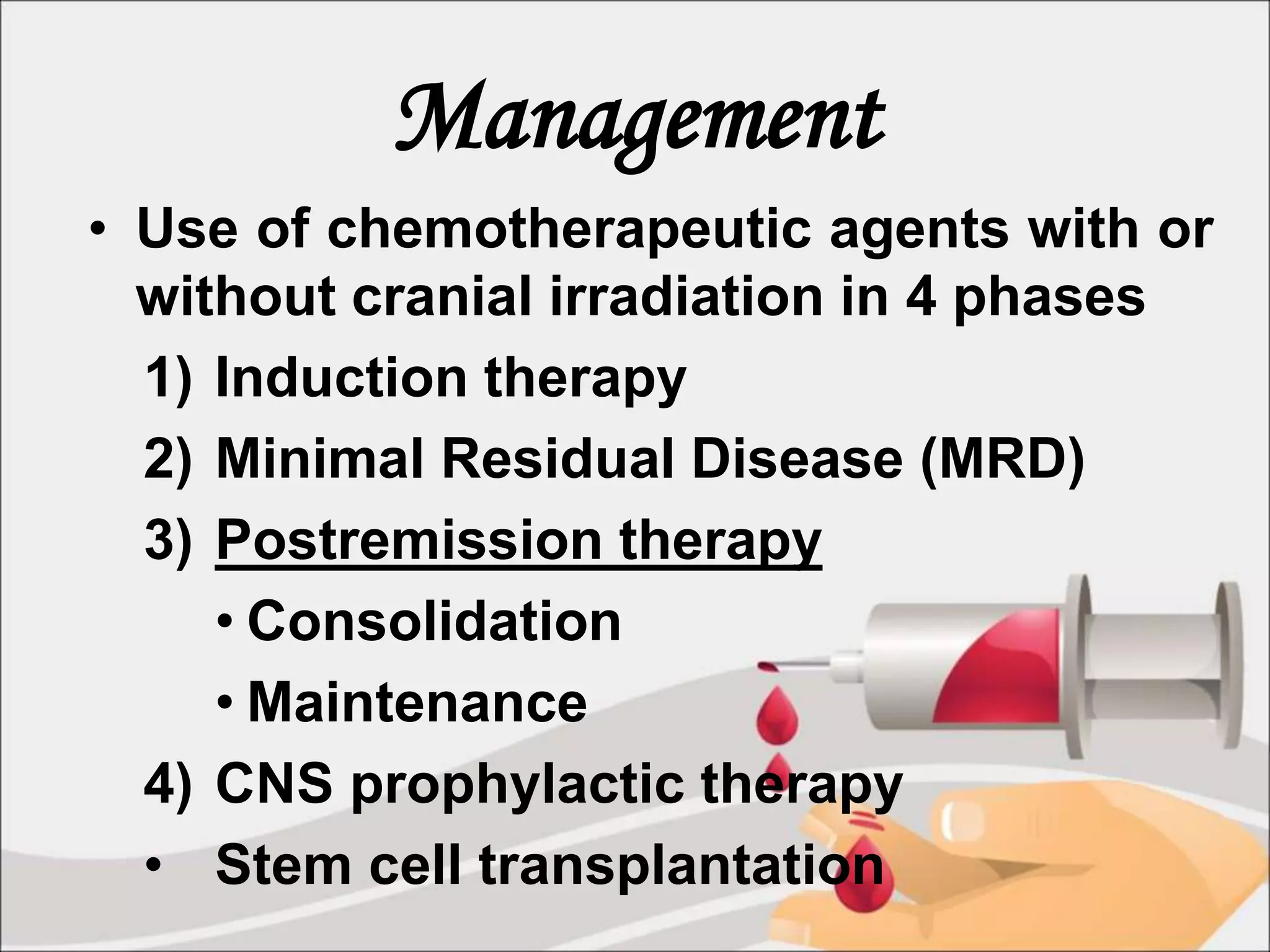
The document discusses childhood leukemia, describing it as cancer that affects the blood and bone marrow characterized by excessive production of immature white blood cells. It defines the main types of leukemia as acute lymphocytic leukemia, acute myeloid leukemia, chronic lymphocytic leukemia, and chronic myeloid leukemia. The document also outlines the diagnostic evaluation and management of childhood leukemia, including induction therapy, consolidation therapy, maintenance therapy, and stem cell transplantation.