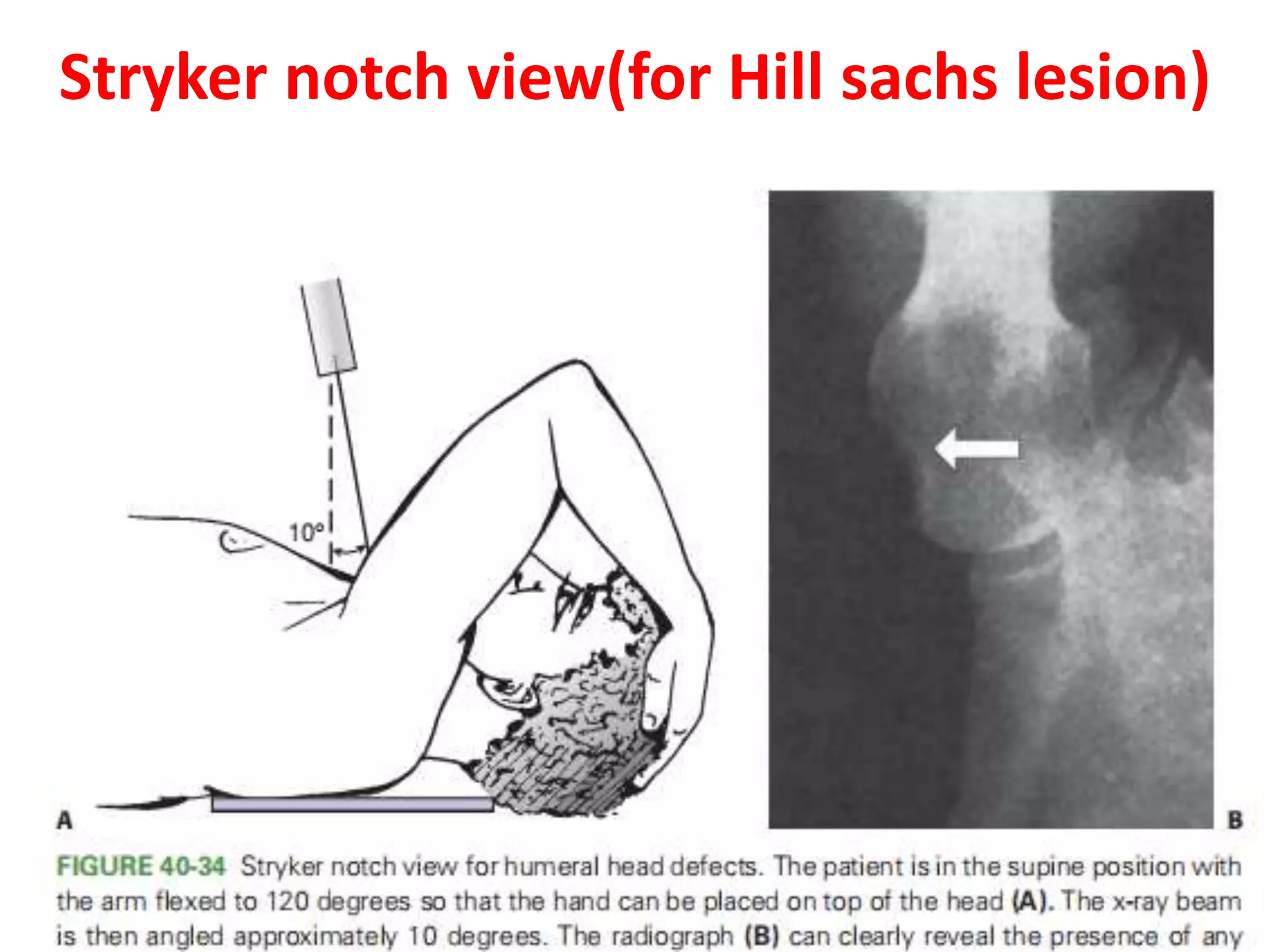
A 60-year-old woman with a left anterior shoulder dislocation following a fall presented with pain and limited movement. Examination and imaging reveal potential rotator cuff tears and other complications, leading to various treatment options such as closed reduction, open reduction, or arthroplasty depending on her condition and the age of the dislocation. Post-operative management includes rehabilitation strategies tailored to her specific needs and recovery progress.