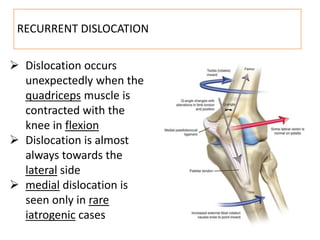
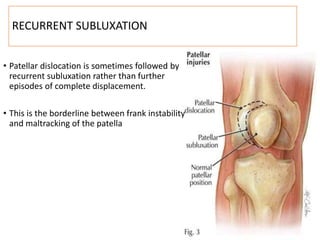
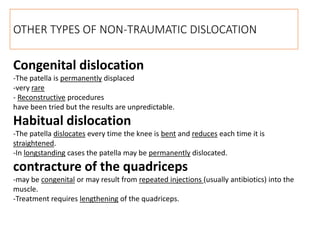
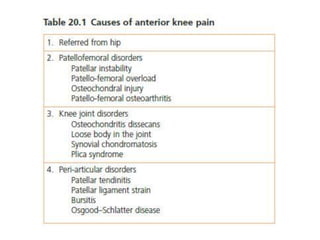
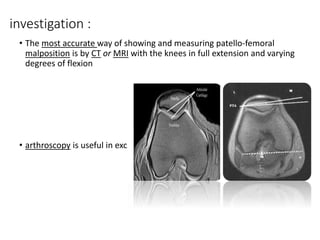
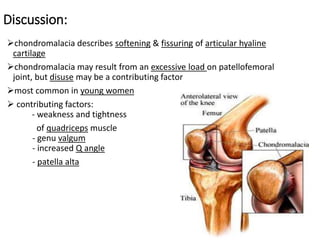
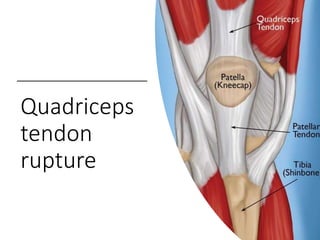
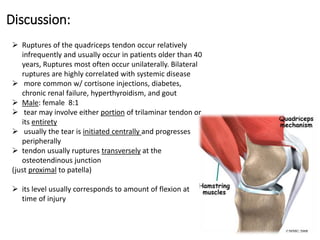
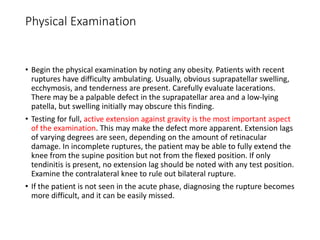
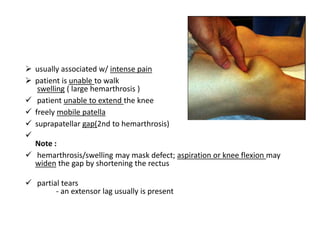
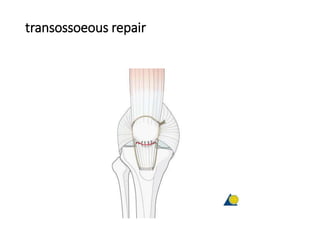
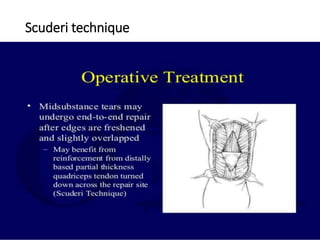
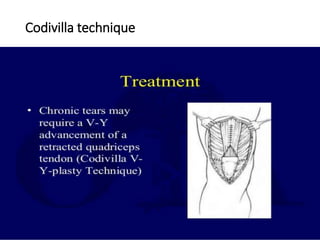
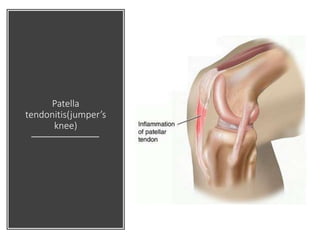
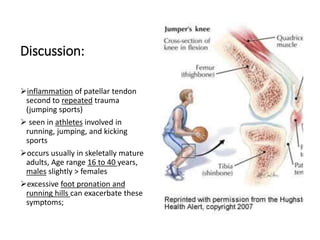
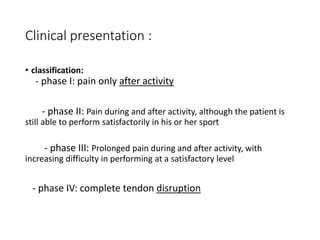
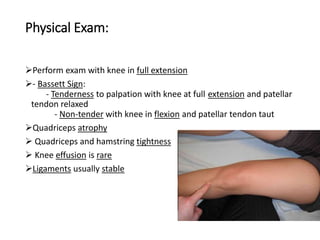
This document summarizes knee disorders including patellar instability, lateral patellar compression syndrome, idiopathic chondromalacia patellae, quadriceps tendon rupture, and patella tendon tendinitis. It describes the causes, clinical presentations, physical exam findings, and treatment options for each condition. Quadriceps tendon rupture most often occurs in patients over 40 years old and is usually caused by an eccentric contraction of the quadriceps muscle with the foot planted and knee partially flexed. Physical exam may reveal swelling, ecchymosis, and a palpable defect in the suprapatellar region.