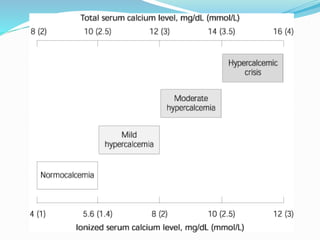
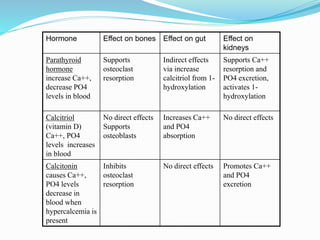
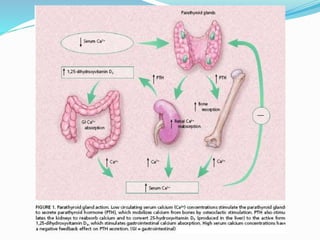
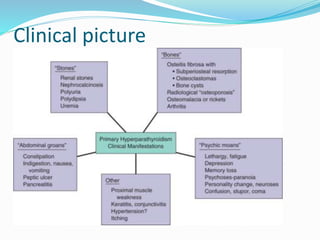
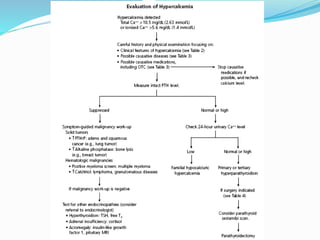
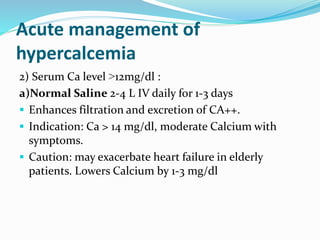
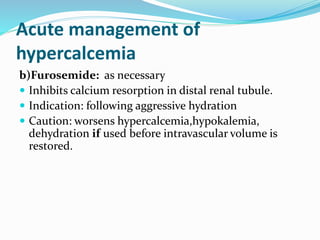
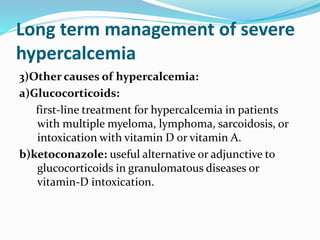
This document defines hypercalcemia and discusses its causes, evaluation, clinical presentation, and management. The main causes are parathyroid hormone dependent (primary hyperparathyroidism, tertiary hyperparathyroidism) and independent (malignancy, vitamin D related, endocrinopathies). Evaluation involves history, exam, and labs. Acute management is rehydration and medications to increase calcium excretion. Long term management depends on the underlying cause and may involve surgery, bisphosphonates, glucocorticoids, or ketoconazole.