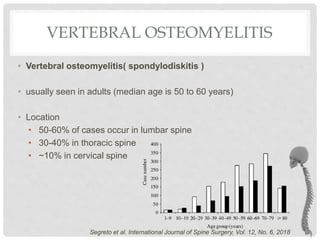
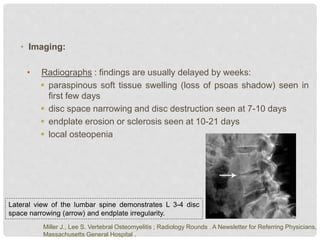
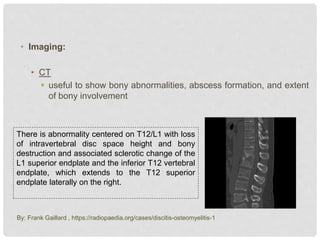
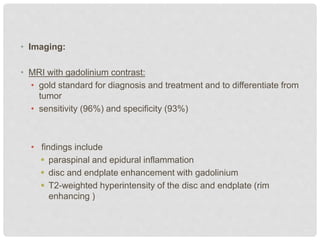
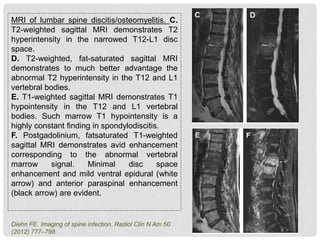
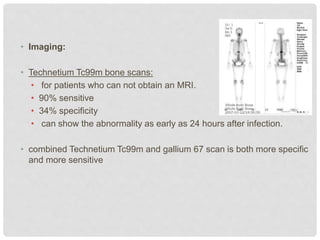
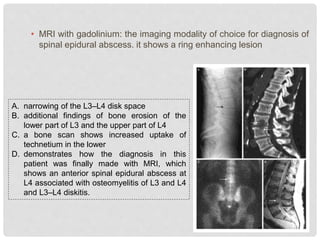
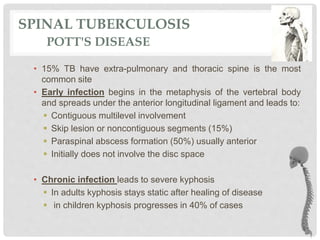
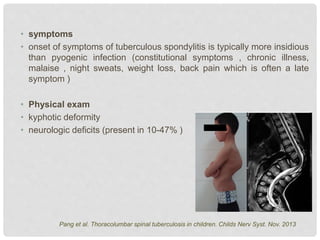
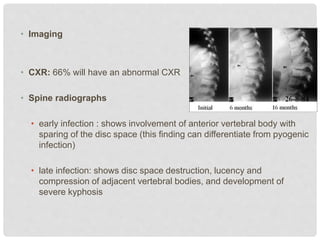
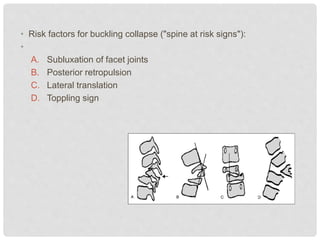
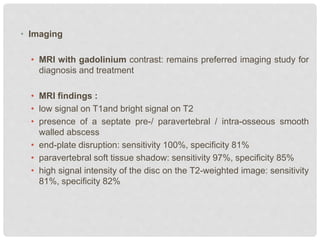
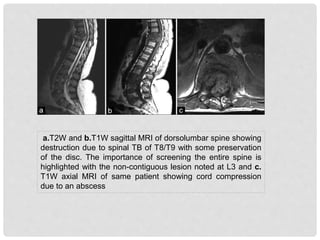
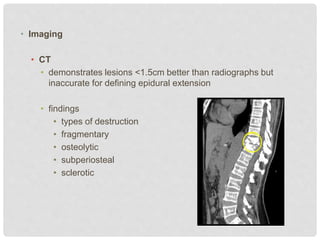
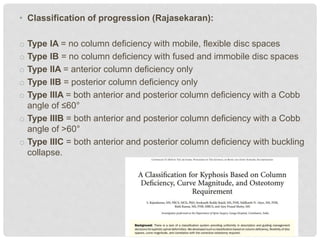
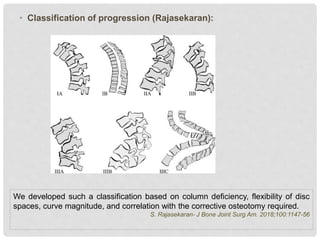
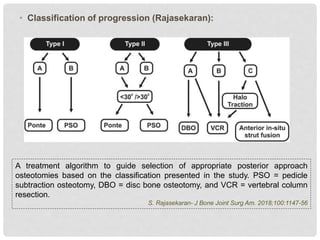
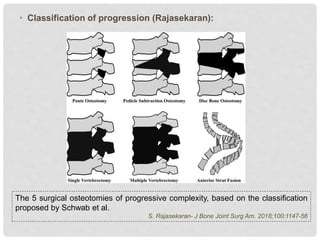
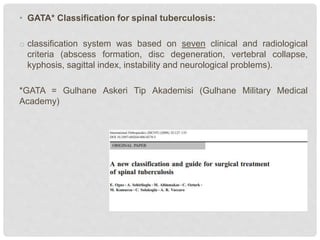
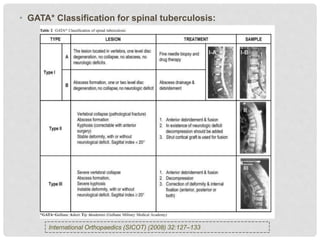
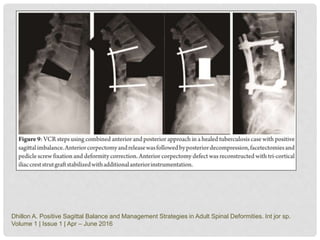
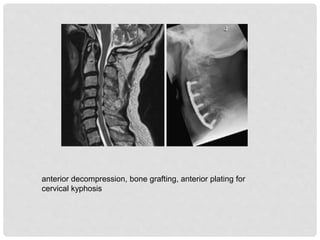
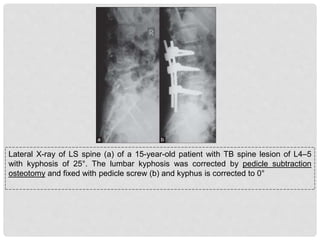
The document discusses vertebral osteomyelitis, focusing on its epidemiology, risk factors, clinical presentation, and imaging techniques for diagnosis. It highlights non-operative and operative treatment options, including the significance of antibiotic therapy and surgical interventions for severe cases. Additionally, it covers spinal tuberculosis, its diagnosis, classifications, and treatment modalities, emphasizing the complexities involved in managing these conditions.