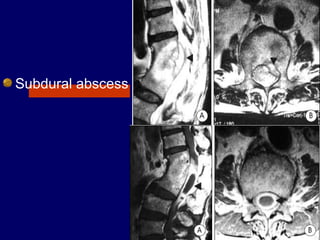
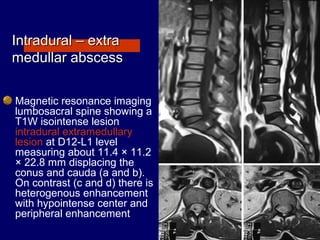
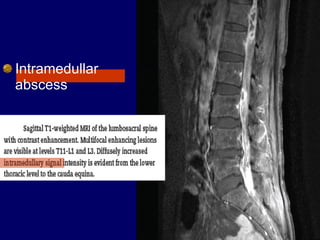
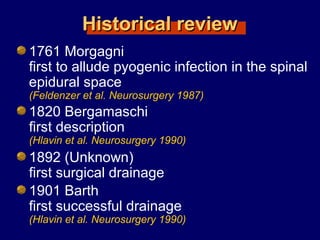
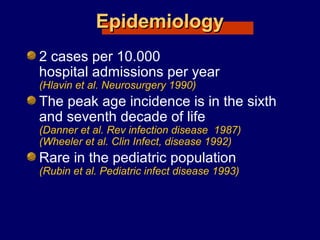
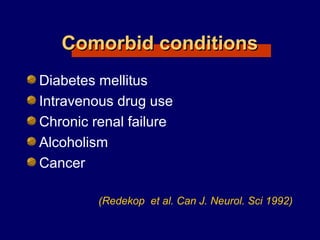
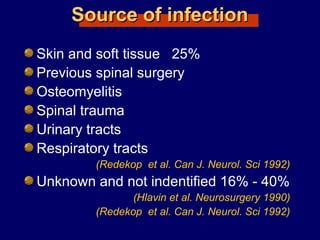
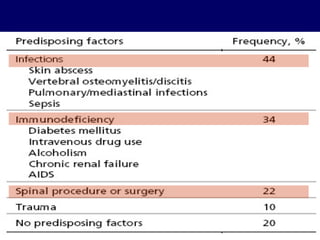
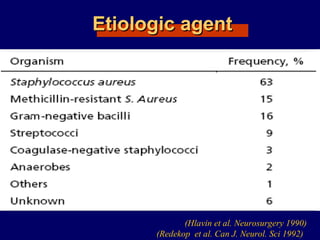
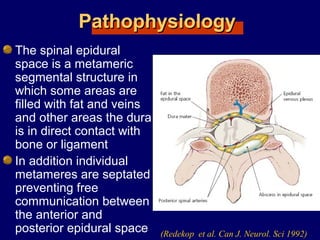
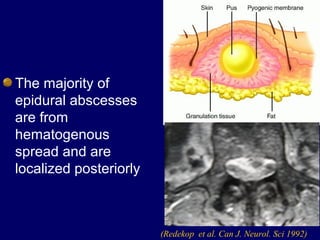
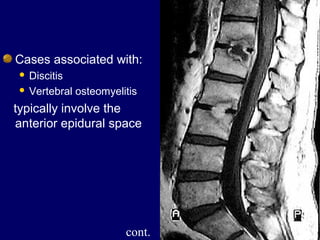
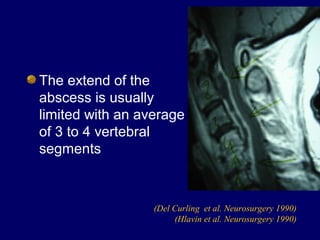
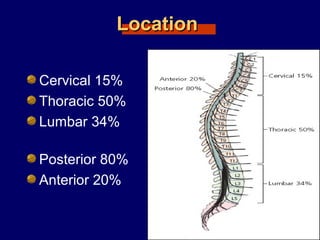
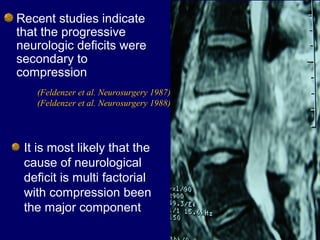
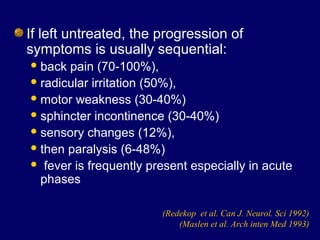
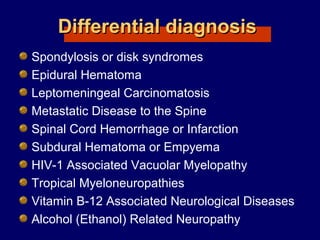
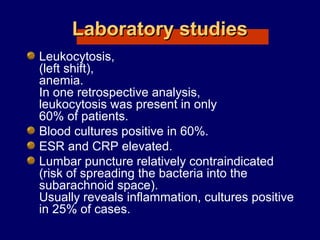
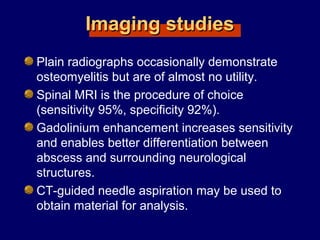
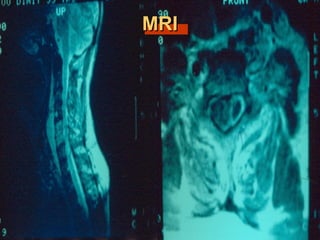
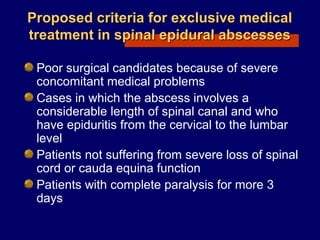
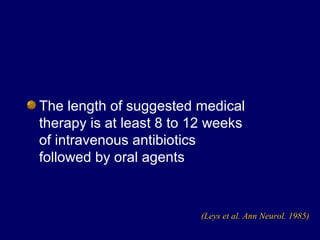
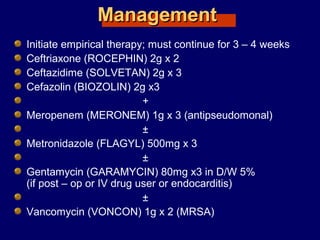
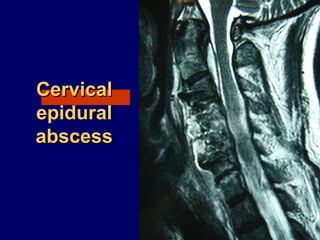
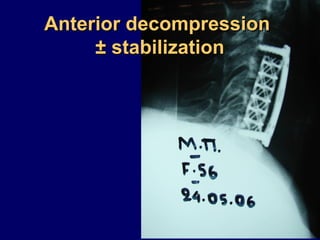
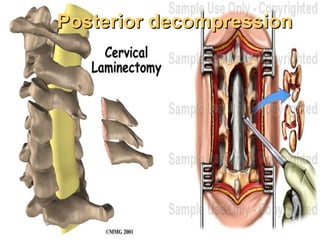
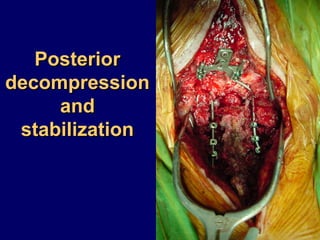
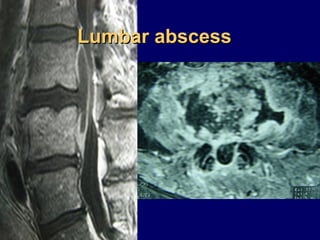
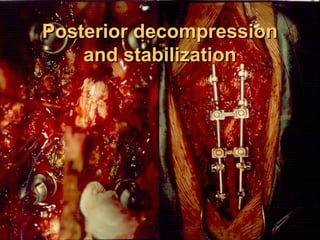
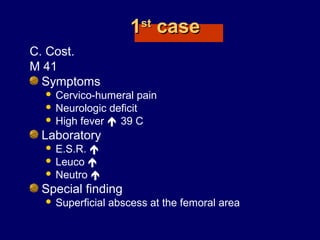
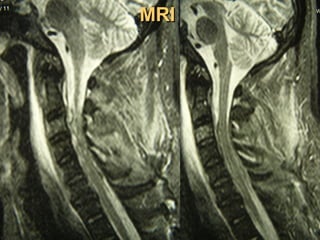
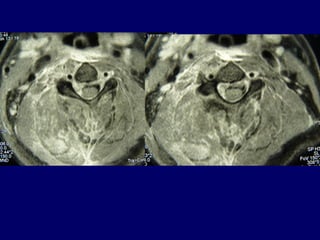
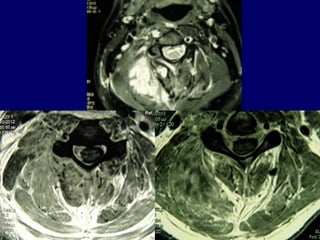
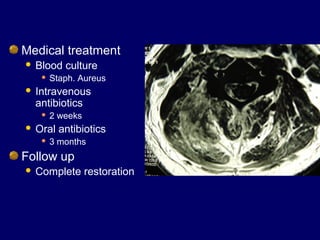
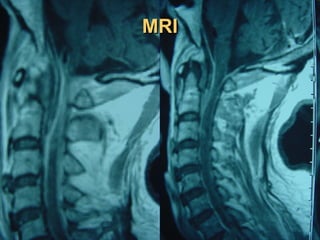
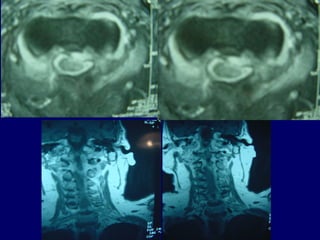
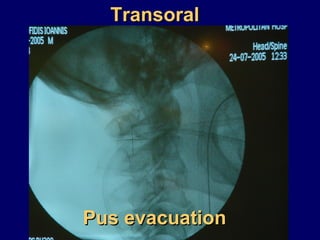
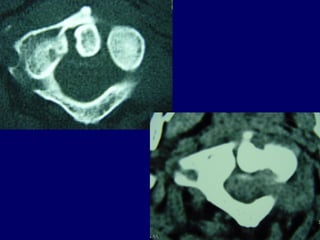
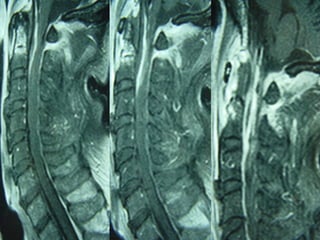
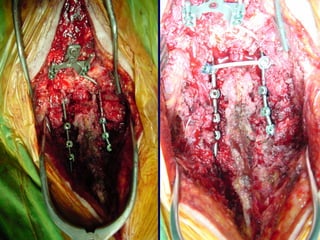
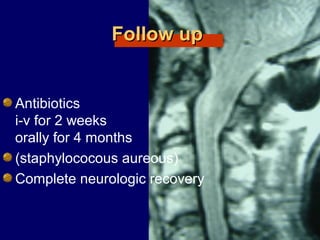
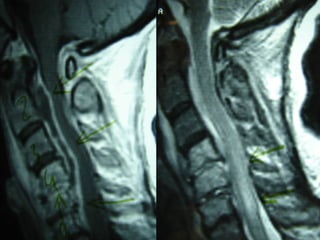
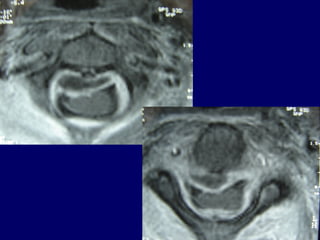
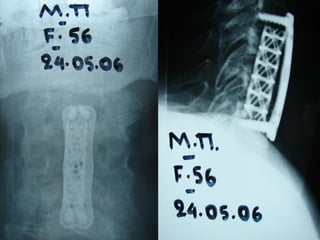
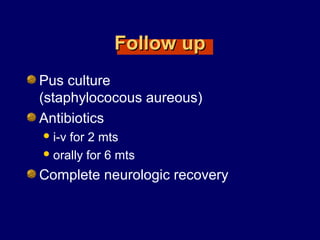
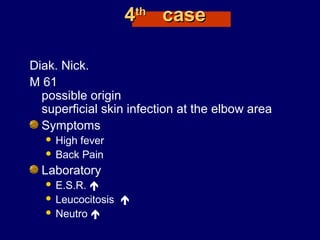
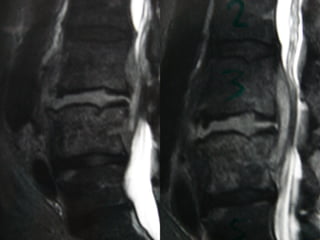
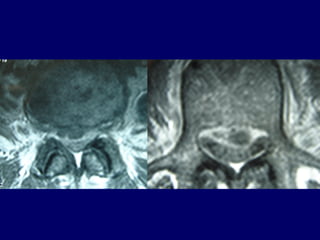
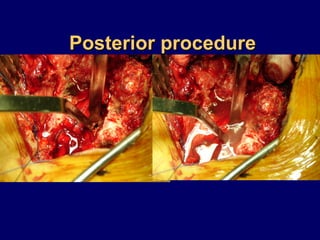
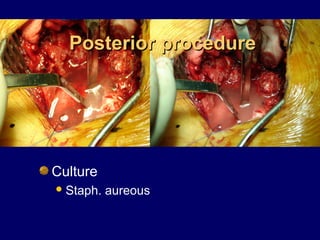
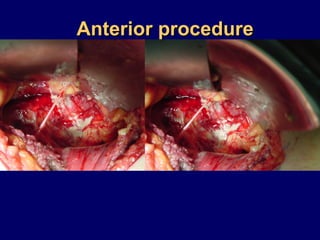
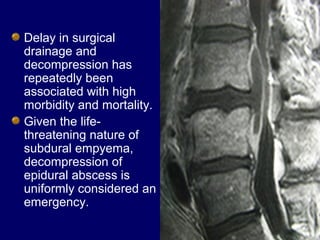
The document discusses spinal abscesses, including epidural and subdural varieties, detailing their epidemiology, pathophysiology, diagnosis, and treatment options. It highlights the importance of early identification and surgical intervention to prevent neurological deficits and complications, as mortality rates can be high if treatment is delayed. The text also provides case studies illustrating various treatment approaches and outcomes for patients with these conditions.