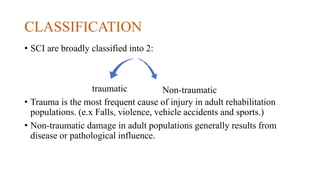
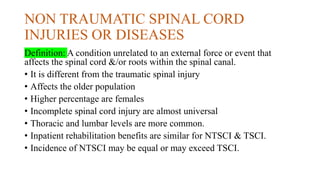
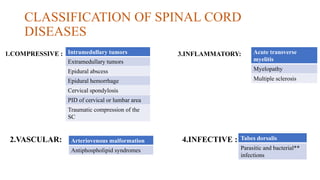
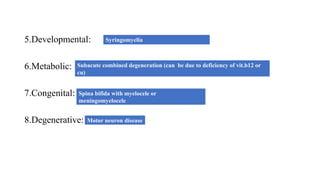
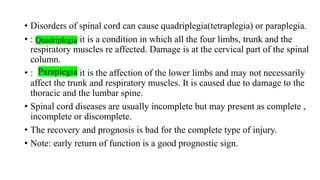
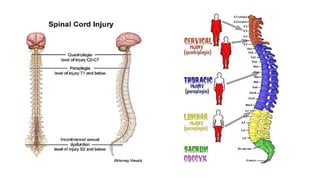
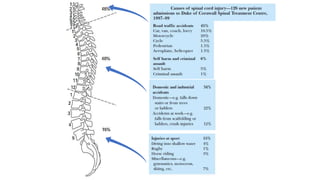
1. Spinal cord injuries and diseases can be traumatic due to external forces or non-traumatic due to underlying conditions. Common non-traumatic diseases include tumors, infections, inflammation, and vascular abnormalities.
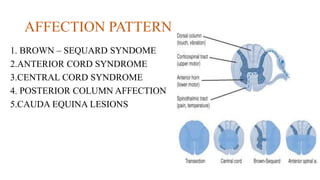
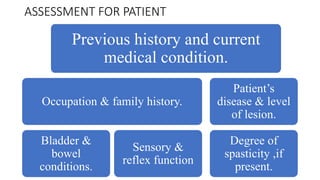
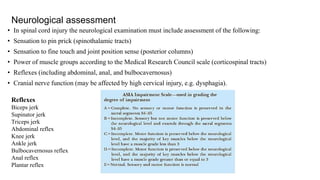
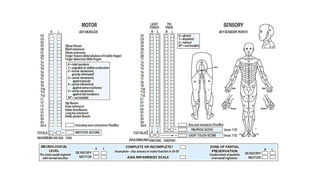
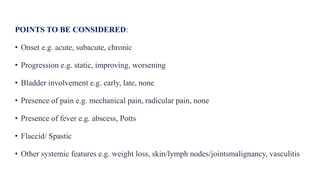
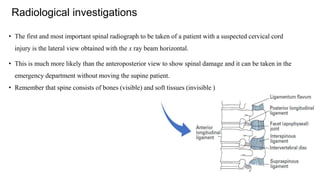
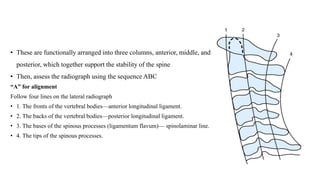
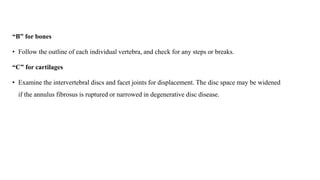
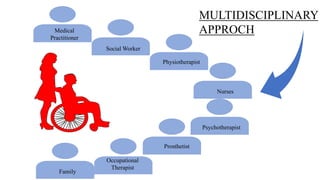
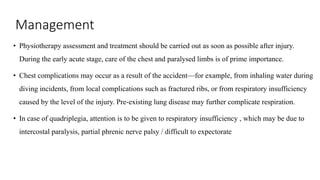
2. Assessment involves evaluating neurological function, imaging like MRI to identify abnormalities, and diagnostic tests like lumbar puncture. Management depends on the specific condition but may require surgery, antibiotics, steroids, or other treatments.
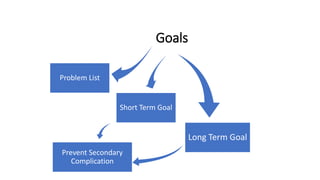
3. Outcomes depend on the level and completeness of injury, with earlier treatment often leading to better recovery of function. Quality of life is significantly impacted due to paralysis and other functional limitations.