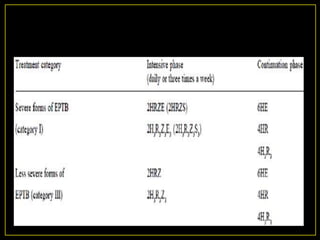
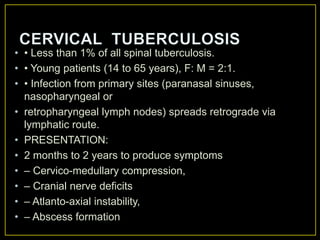
The document discusses spinal tuberculosis, noting that it causes delays in diagnosis, long recovery periods, and high costs. Key points include:
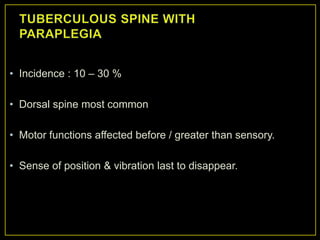
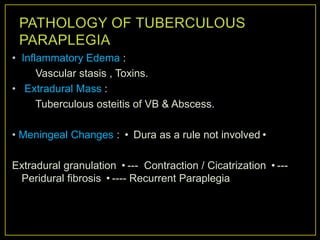
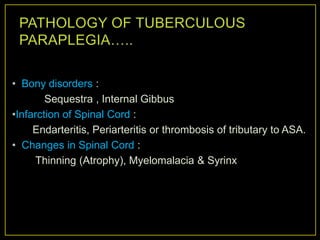
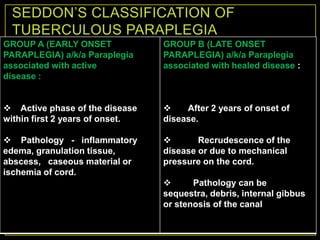
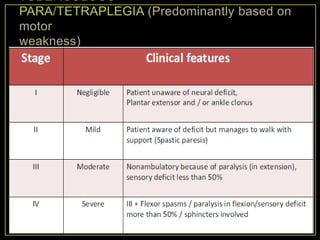
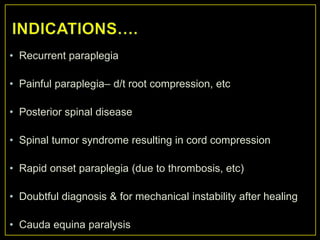
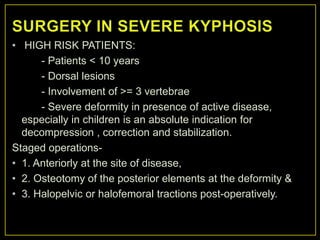
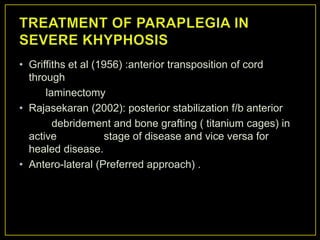
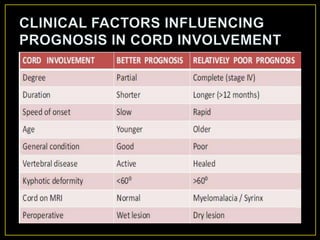
- Paralysis occurs in up to 50% of spinal tuberculosis patients.
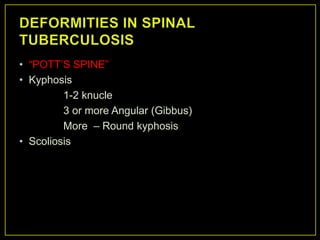
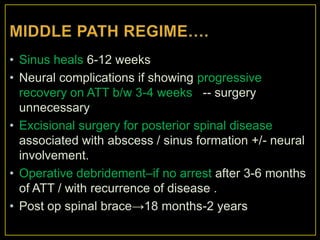
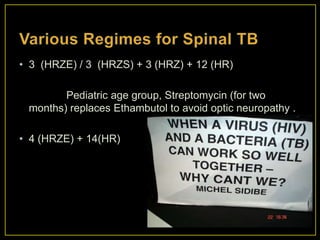
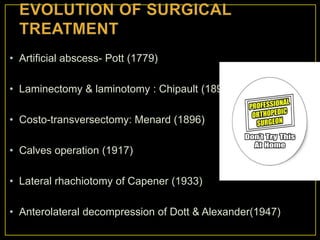
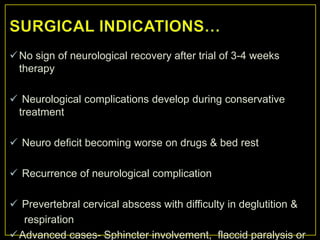
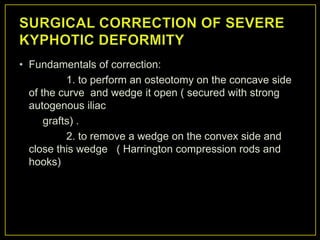
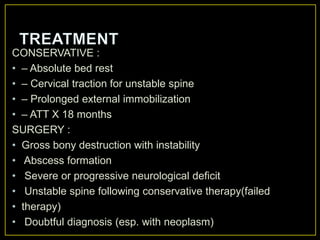
- Early diagnosis, expedient treatment, aggressive surgery, and preventing deformity lead to the best outcomes.
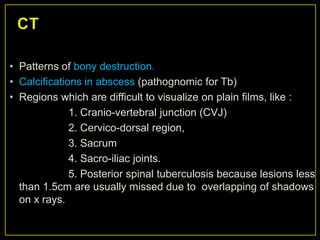
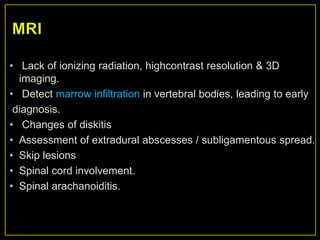
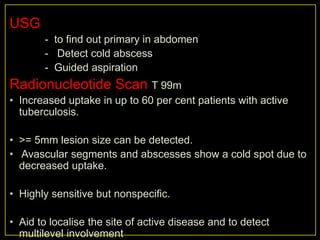
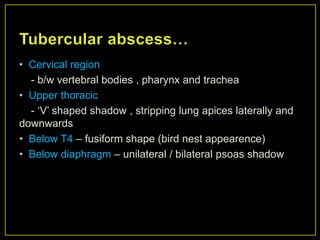
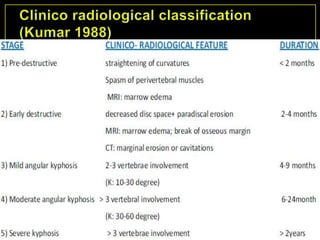
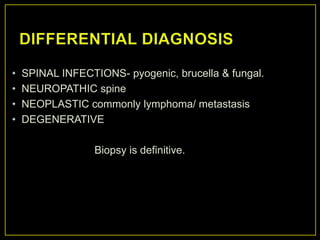
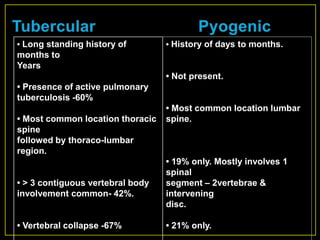
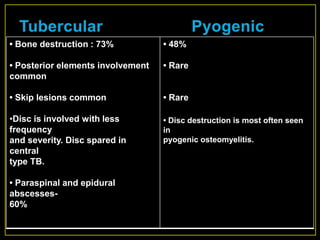
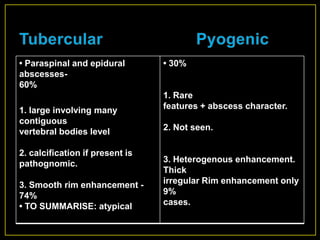
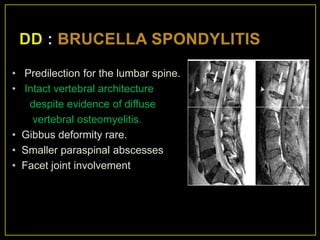
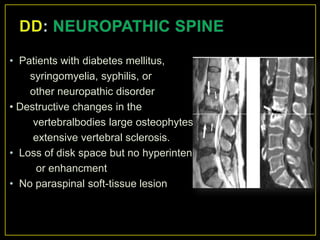
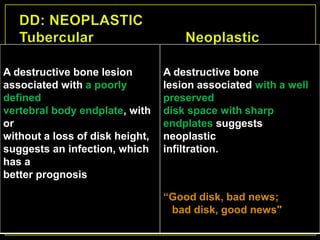
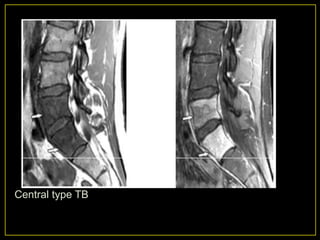
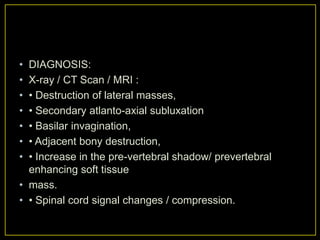
- Diagnosis relies on tests like tuberculin skin tests, imaging like MRI to identify bone destruction and abscesses, and microscopy and culture of samples.
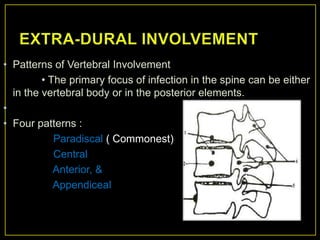
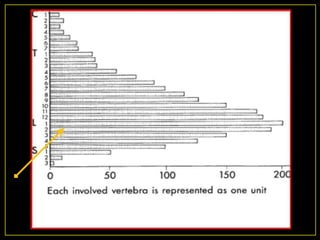
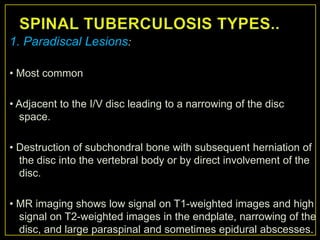
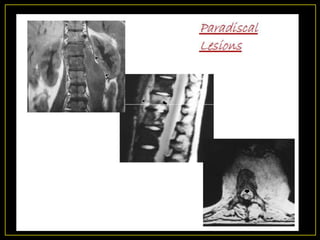
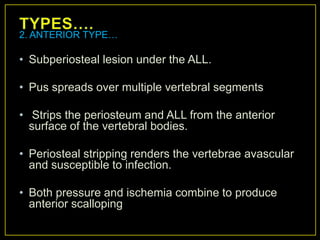
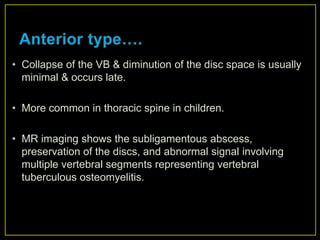
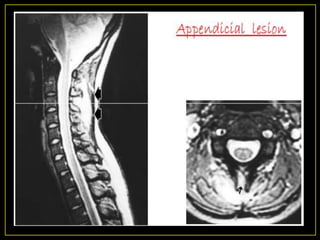
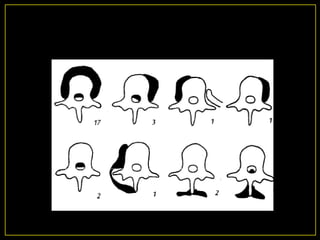
- Patterns of bone involvement include paradiscal, central, anterior, and appendiceal lesions.
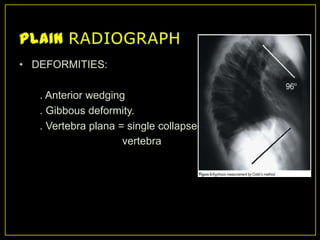
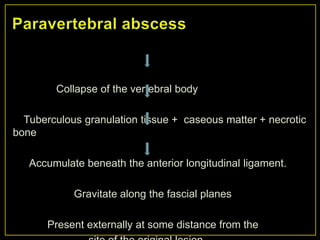
- Complications include paralysis, cold abscesses, deformities, and secondary infections.