This document discusses spinal tuberculosis, including:
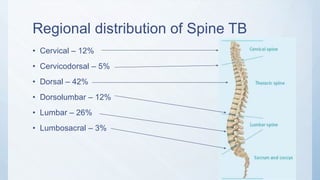
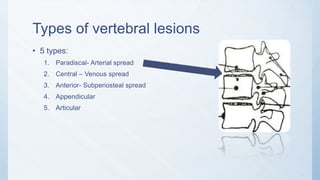
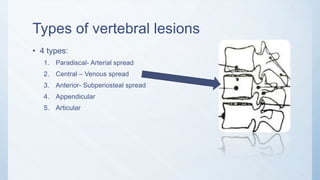
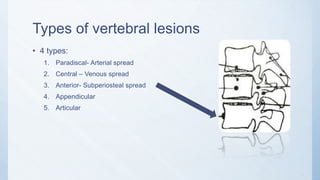
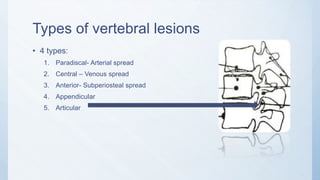
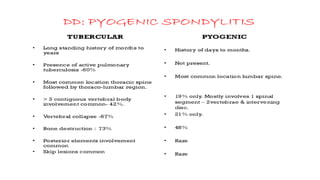
1. It affects the dorsal spine in 42% of cases and describes 4 types of vertebral lesions.
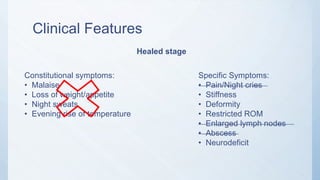
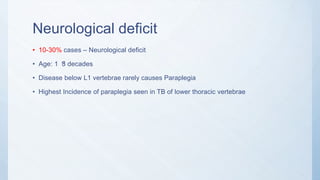
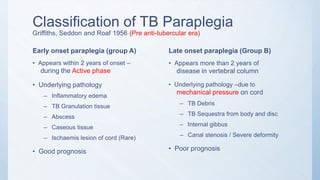
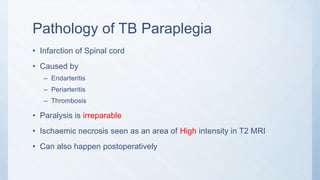
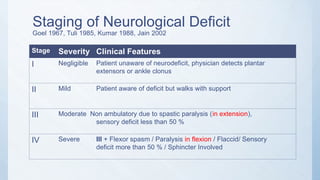
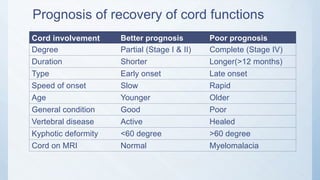
2. Symptoms include back pain, stiffness, and potential neurological deficit in advanced cases.
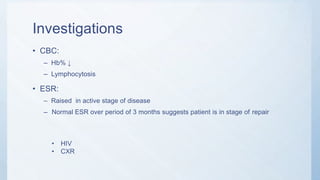
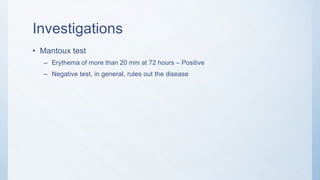
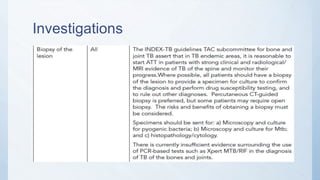
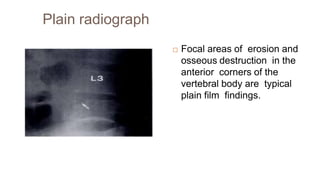
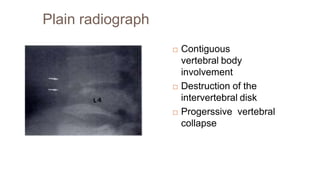
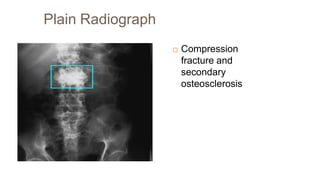
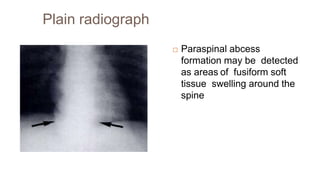
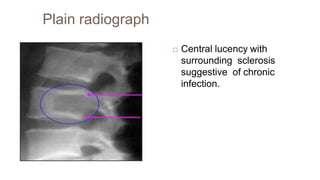
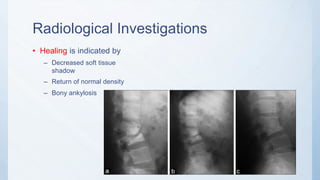
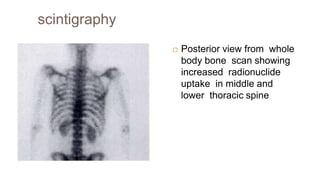
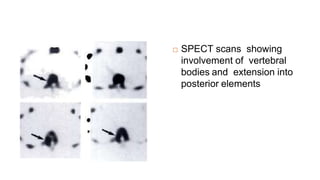
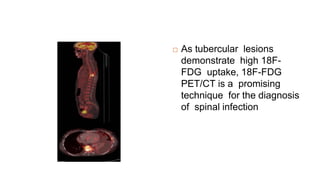
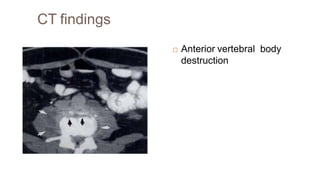
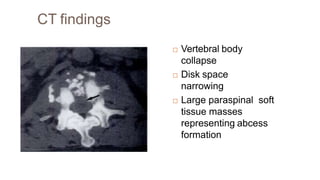
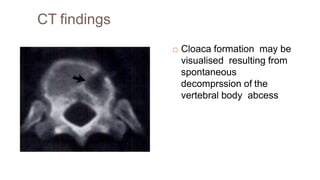
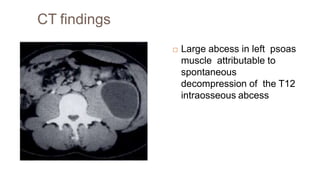
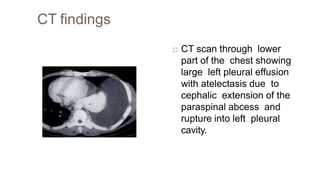
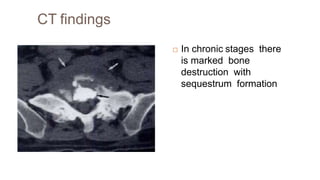
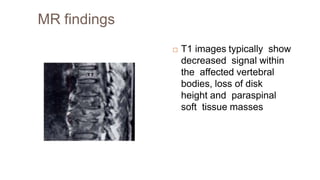
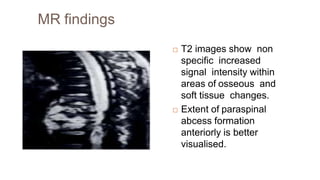
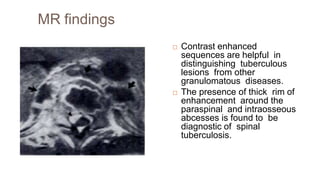
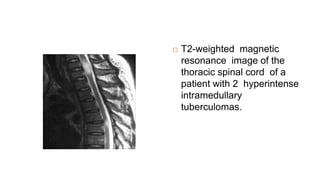
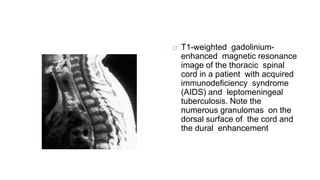
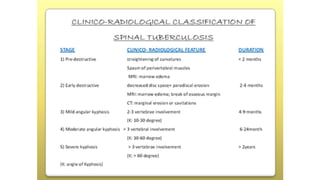
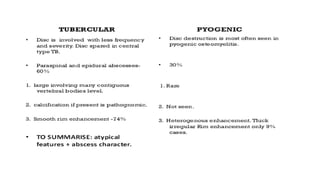
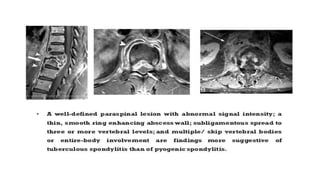
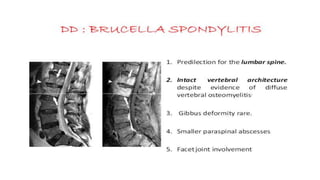
3. Investigations include blood tests, imaging like xray, CT and MRI to determine lesion type and severity.
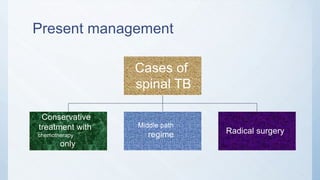
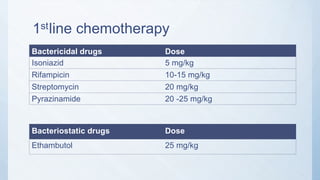
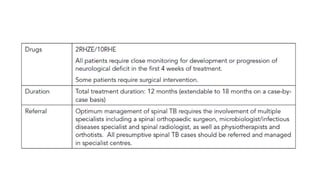
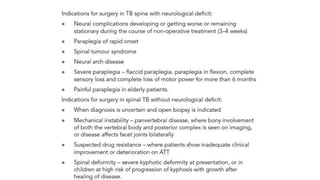
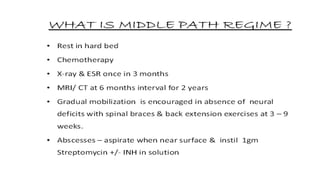
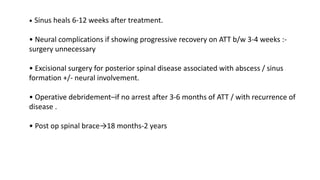
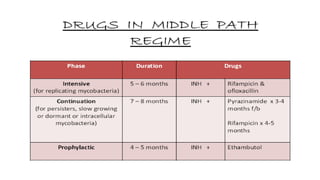
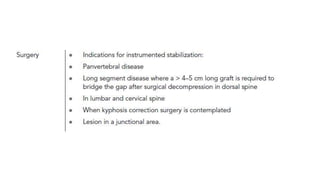
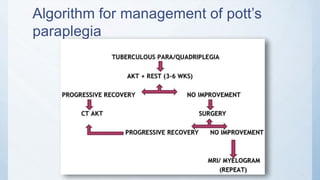
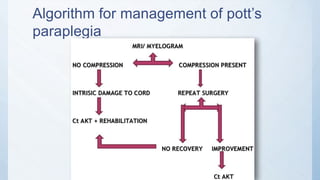
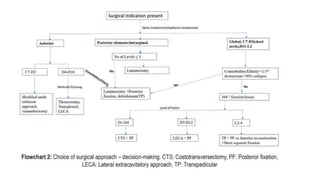
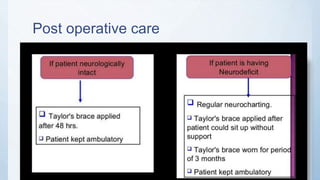
4. Management involves chemotherapy initially but may require surgical intervention for abscesses, severe deformity or neurological deficit.