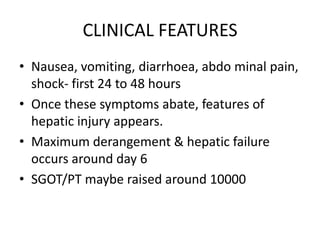
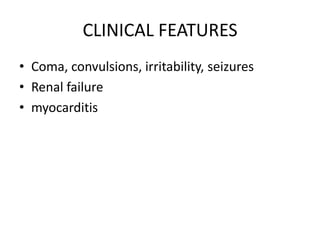
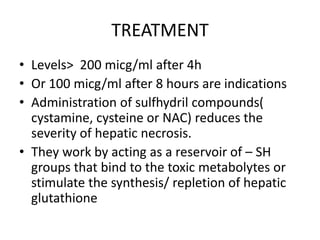
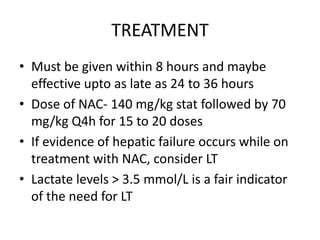
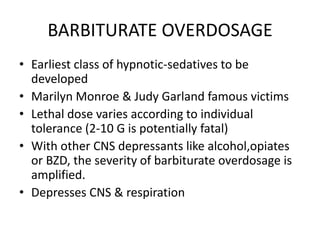
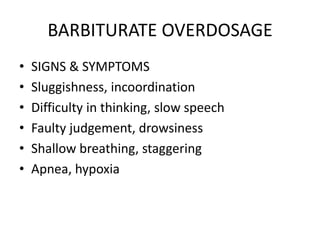
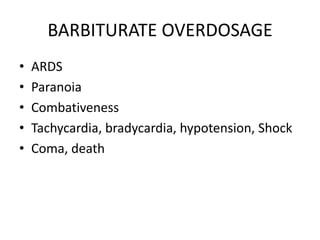
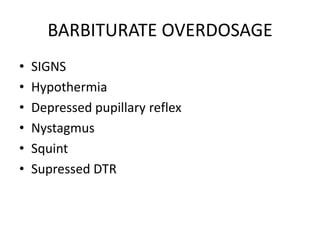
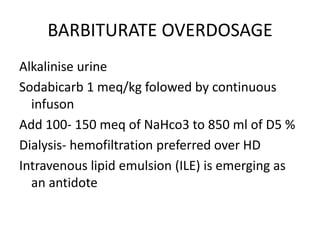
1. Paracetamol and barbiturate overdoses are common causes of acute liver failure and can be fatal at high doses. N-acetylcysteine treatment may help if given within 24 hours of ingestion.
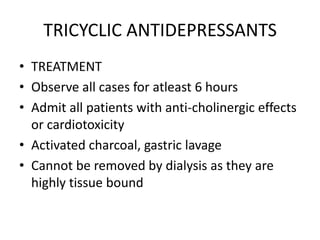
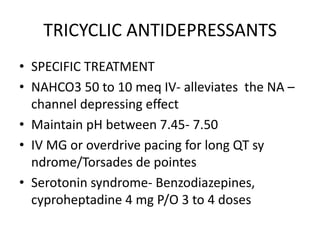
2. Tricyclic antidepressant overdoses can cause seizures, cardiac toxicity, and serotonin syndrome due to their anticholinergic and sodium channel blocking effects. Treatment involves monitoring, sodium bicarbonate, and overdrive pacing or magnesium for cardiac issues.
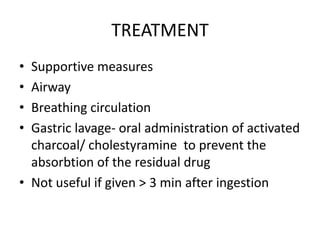
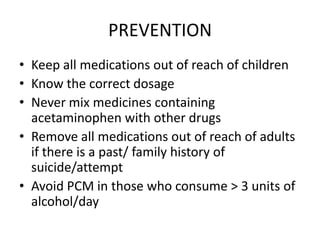
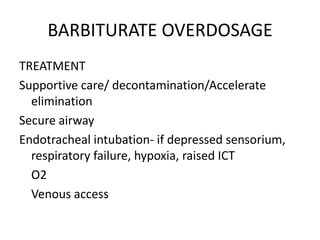
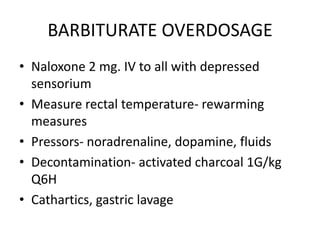
3. Prompt supportive care including airway management and decontamination measures are important for managing overdoses of these common drugs to prevent complications and death.