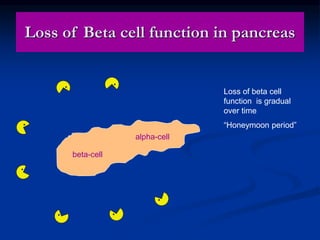
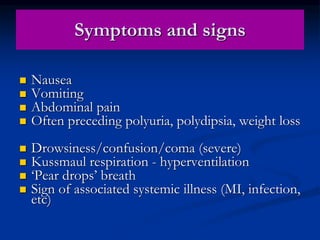
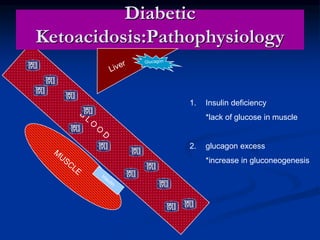
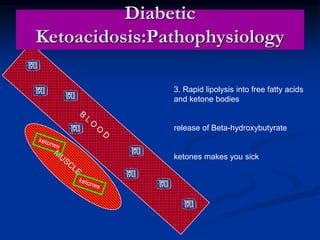
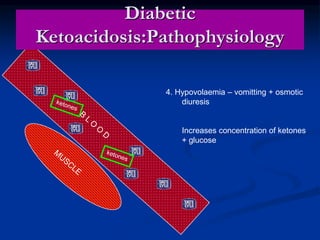
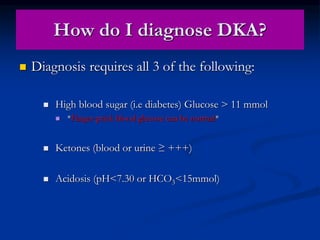
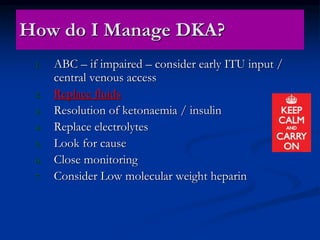
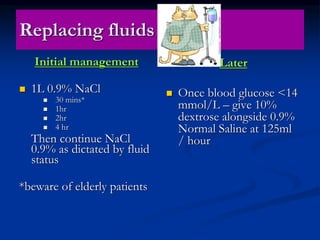
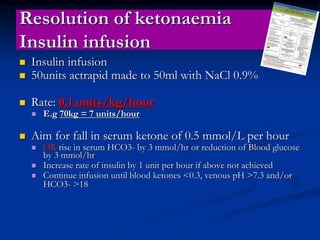
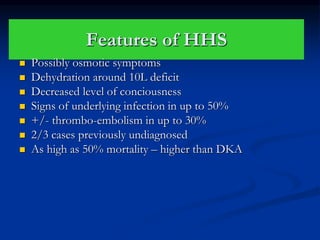
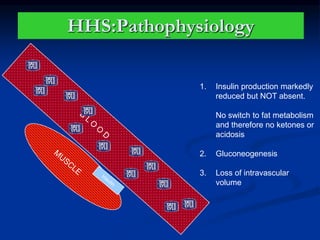
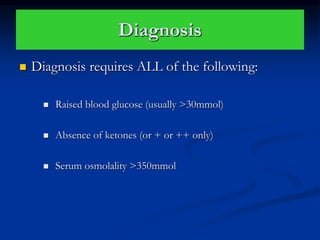
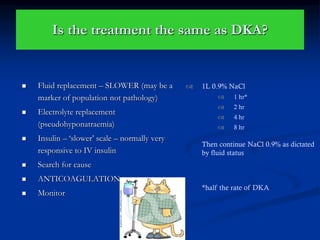
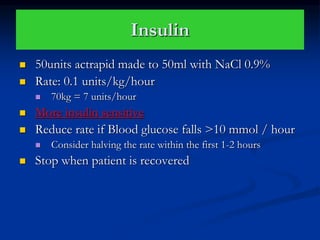
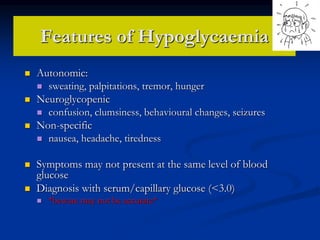
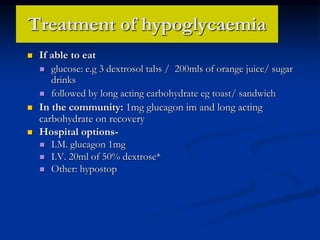
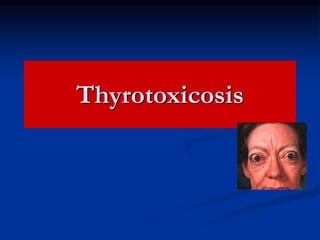
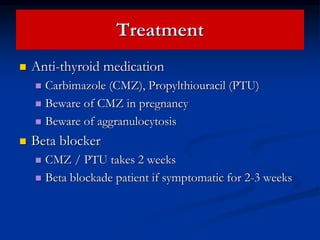
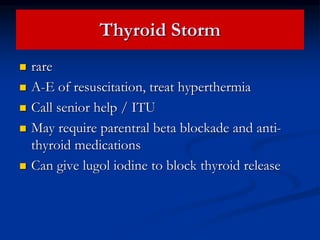
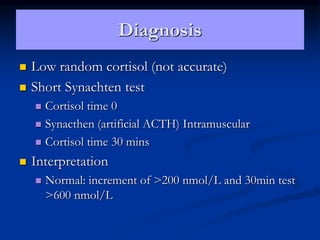
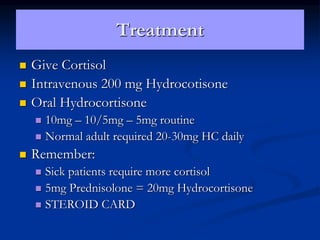
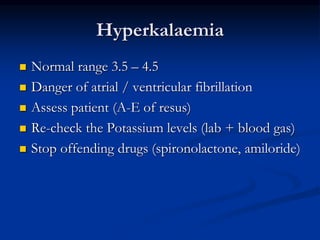
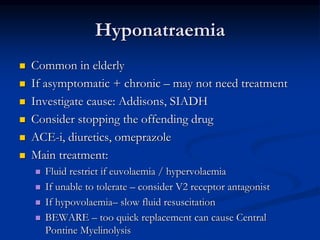
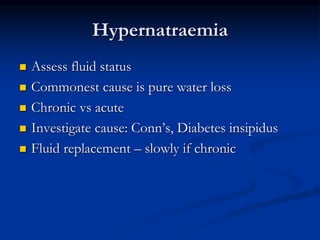
This document provides an overview of endocrine emergencies, including diabetic emergencies like diabetic ketoacidosis and hypoglycemia. It also covers other metabolic disorders such as thyrotoxicosis, Addisonian crisis, and electrolyte abnormalities. For each condition, it describes the symptoms, pathophysiology, diagnosis, and treatment approach. The goal is to help recognize and initiate management of these urgent endocrine conditions.