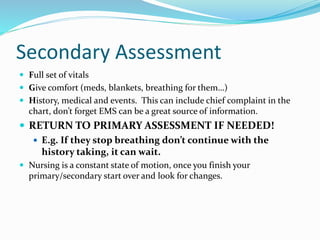
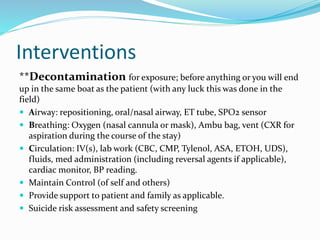
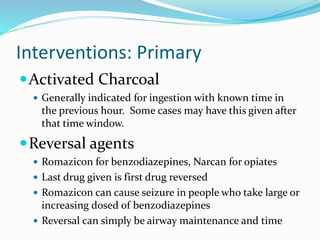
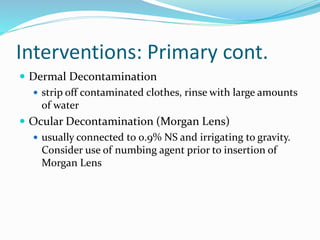
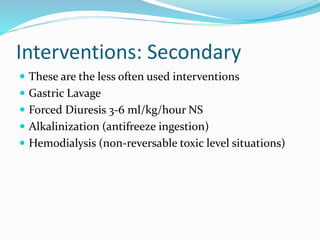
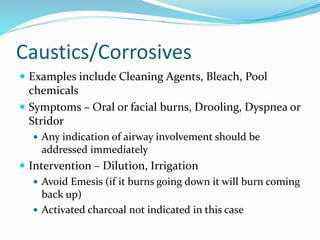
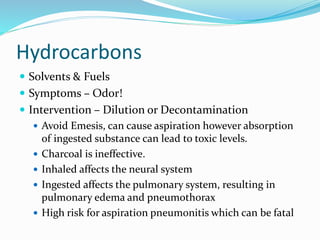
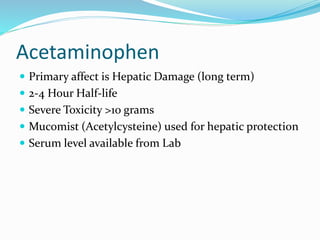
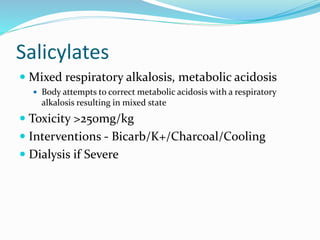
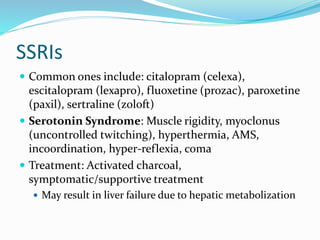
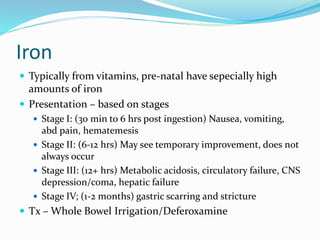
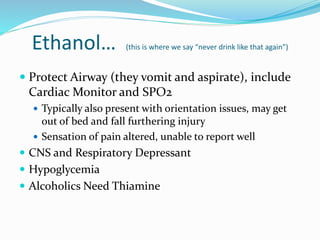
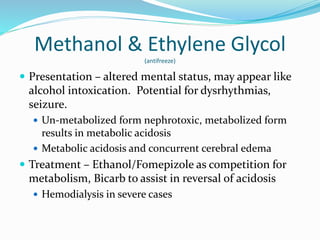
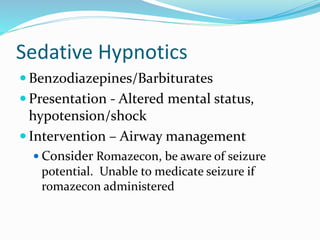
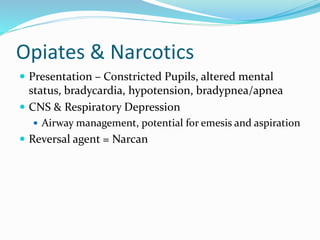
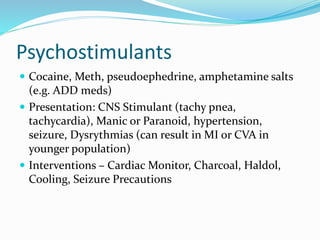
The document provides information on poisonings and toxicology in the emergency department setting. It discusses that approximately 48% of poison exposure calls involve young children under 5 years old, with poisonings in this age group usually being unintentional. It then outlines key questions to ask patients regarding toxic exposures and summarizes the pathophysiology of different types of toxins, including their effects on the sympathetic, parasympathetic, and central nervous systems. The document concludes by describing primary and secondary patient assessments, various medical interventions for different toxin classes, and considerations for specific toxins like acetaminophen, salicylates, antidepressants, ethanol, and drugs of abuse.