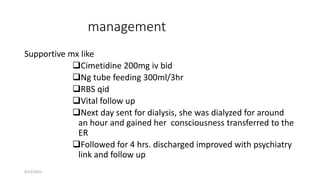
A 17-year-old female presented with loss of consciousness after ingesting 8 grams of carbamazepine tablets. She was comatose on examination. After supportive care including cimetidine, tube feeding, and dialysis, her mental status improved and she was discharged. Carbamazepine toxicity can cause seizures, arrhythmias, respiratory depression, and coma. Treatment involves supportive care, activated charcoal, and enhanced elimination methods like hemodialysis for severe cases.