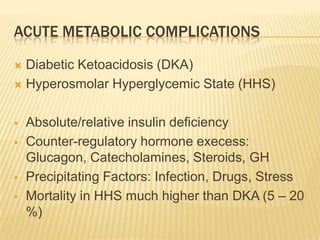
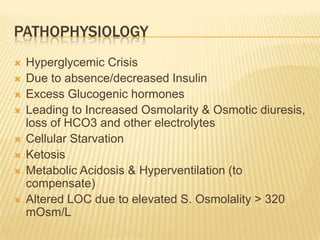
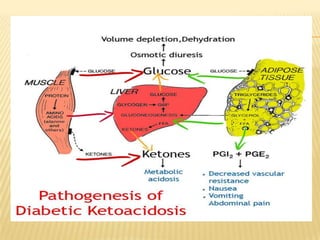
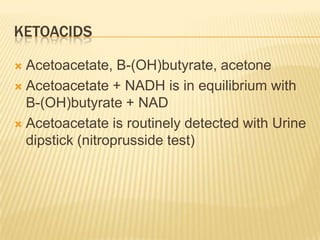
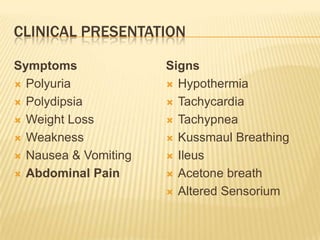
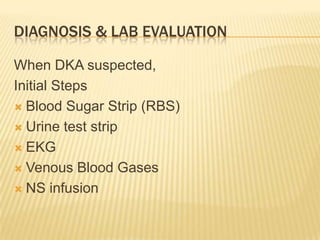
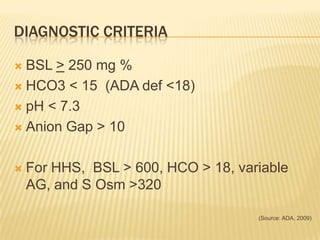
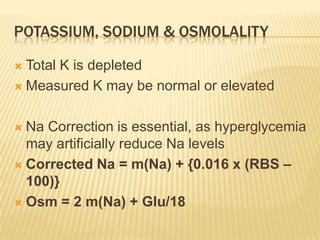
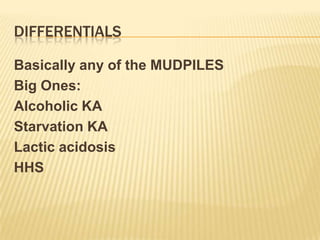
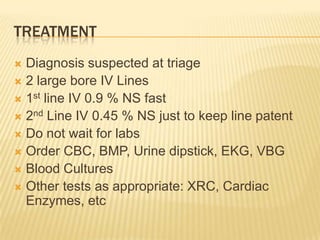
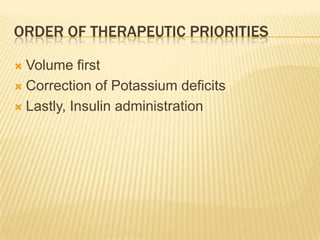
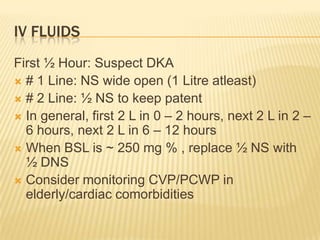
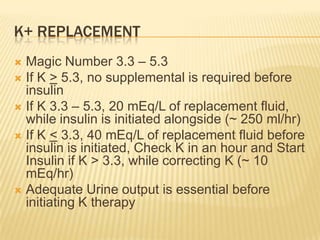
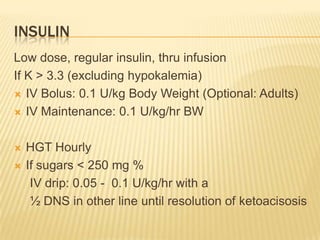
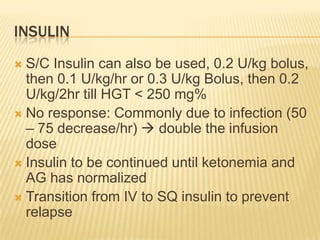
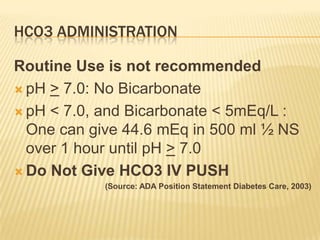
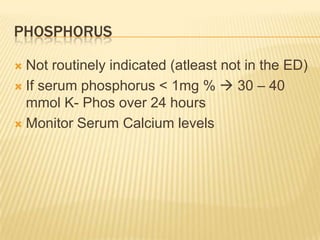
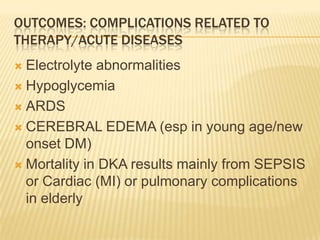
This document discusses diabetic emergencies, specifically diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS). It covers the pathophysiology, clinical presentation, diagnosis, treatment priorities of volume repletion, potassium replacement, and insulin administration, as well as complications, disposition, and pitfalls in management. The goal of treatment is to correct dehydration, electrolyte imbalances, and acidosis while gradually lowering blood glucose levels.