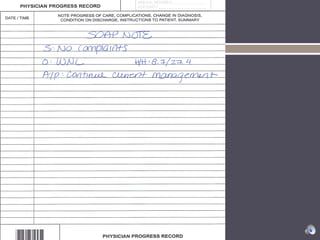
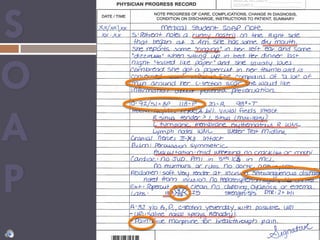
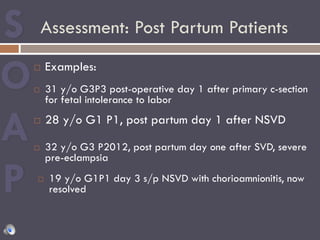
This document provides guidance on writing effective SOAP notes for post-partum patients. It explains that SOAP notes are an important way for healthcare providers to communicate about a patient's condition and care over time. The document reviews the components of the SOAP note format, including the subjective, objective, assessment, and plan sections. It emphasizes that SOAP notes should concisely document the key relevant exam findings and status of the post-partum patient at a moment in time to inform future care.