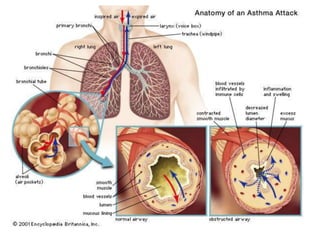
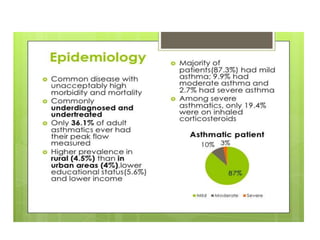
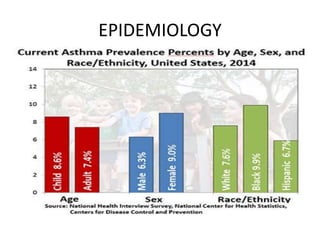
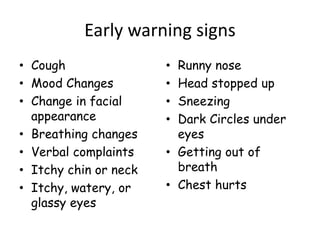
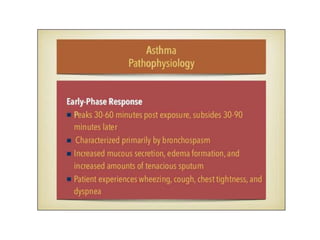
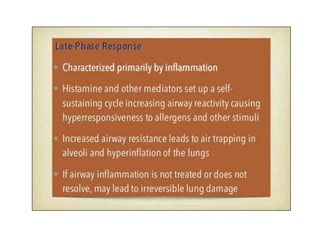
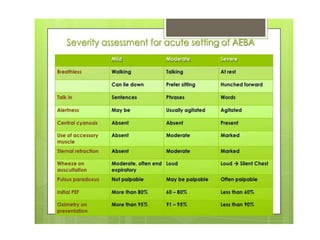
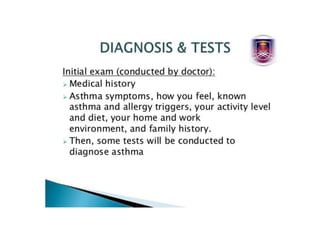
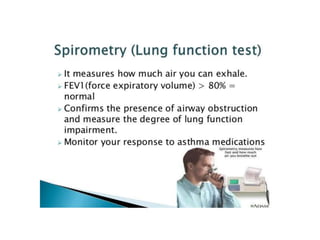
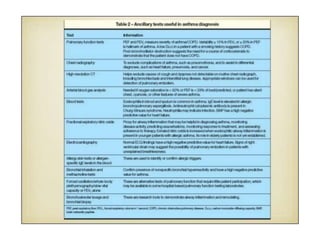
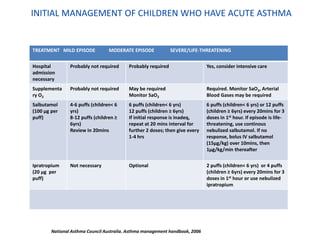
This document provides a comprehensive overview of asthma, detailing its definition, triggers, epidemiology, symptoms, and management strategies, particularly in children. Asthma is characterized as a chronic inflammatory airway disease with various types classified by severity, affecting a significant portion of the population, especially children. Initial management for asthma attacks varies by severity, necessitating different treatments from mild to life-threatening cases.