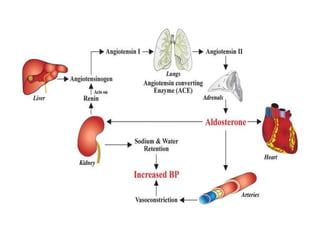
This document summarizes several endocrine emergencies including hypoglycemia, diabetic ketoacidosis, hyperosmolar hyperglycemic nonketotic syndrome, adrenal crisis, pheochromocytoma, thyroid storm, and myxoedema coma. For each condition, it describes the causes, signs and symptoms, investigations, and management principles. The goal of management is resuscitation, treatment of the underlying cause, and stabilization of vital signs and metabolic derangements.