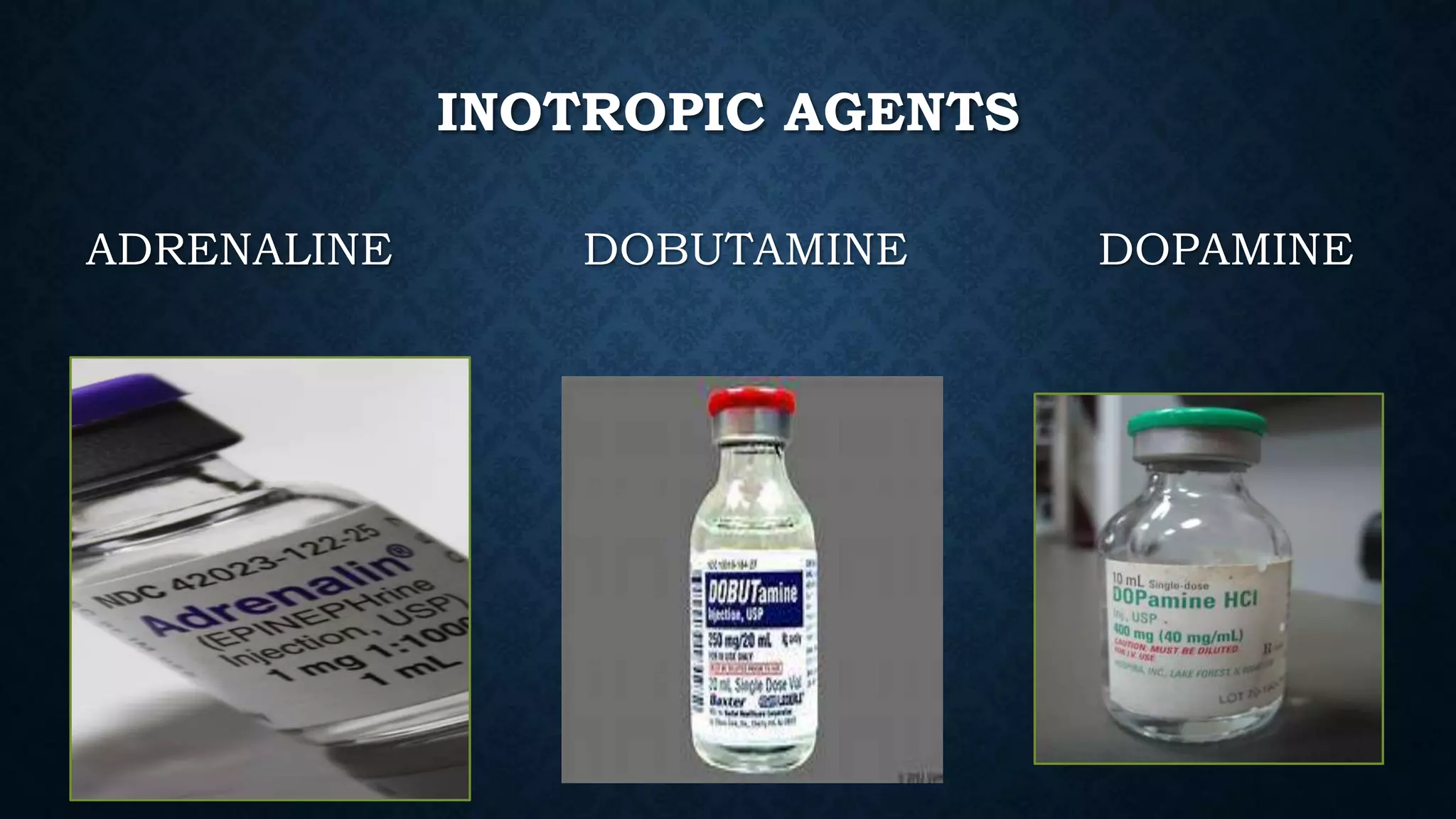
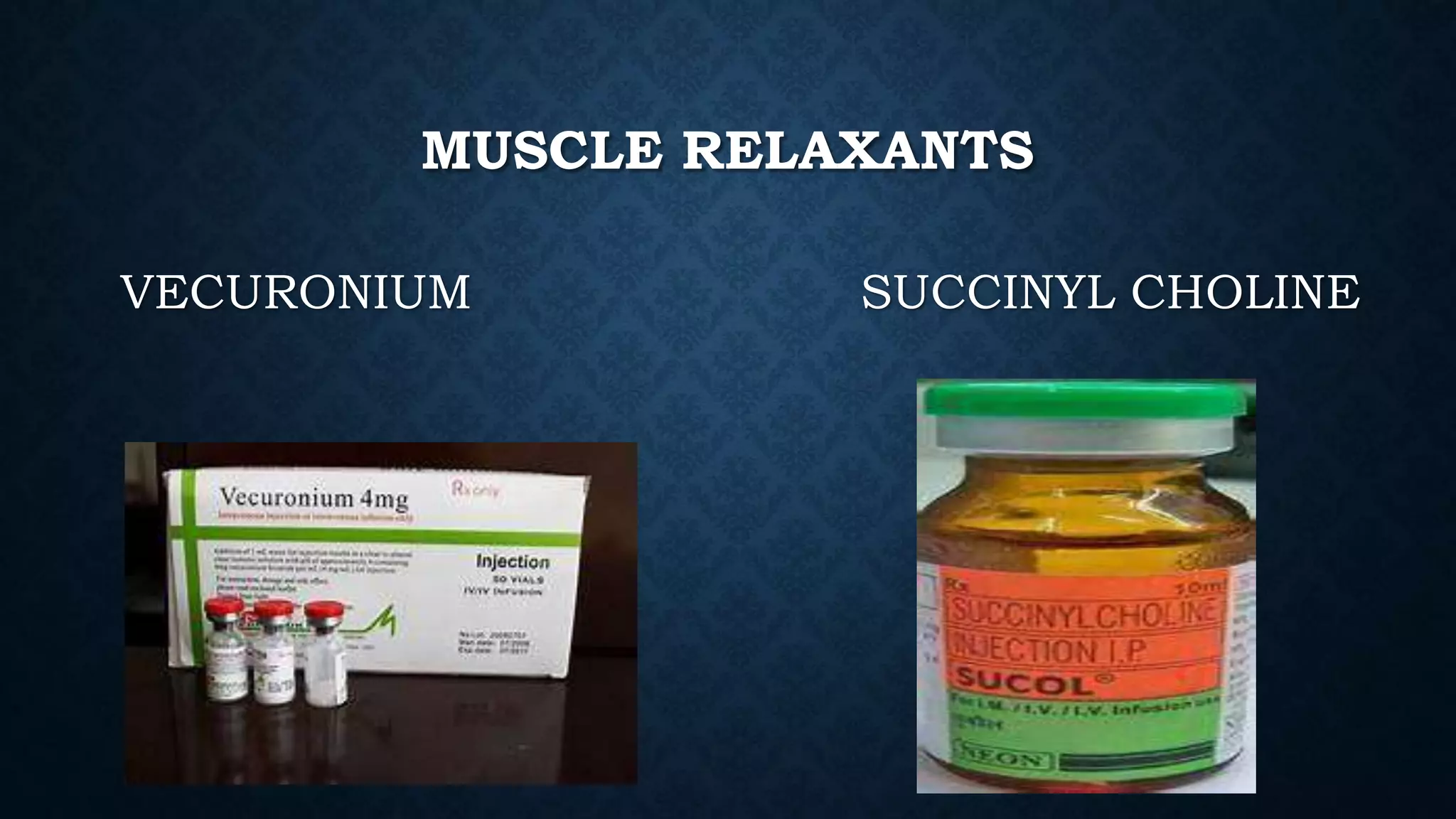
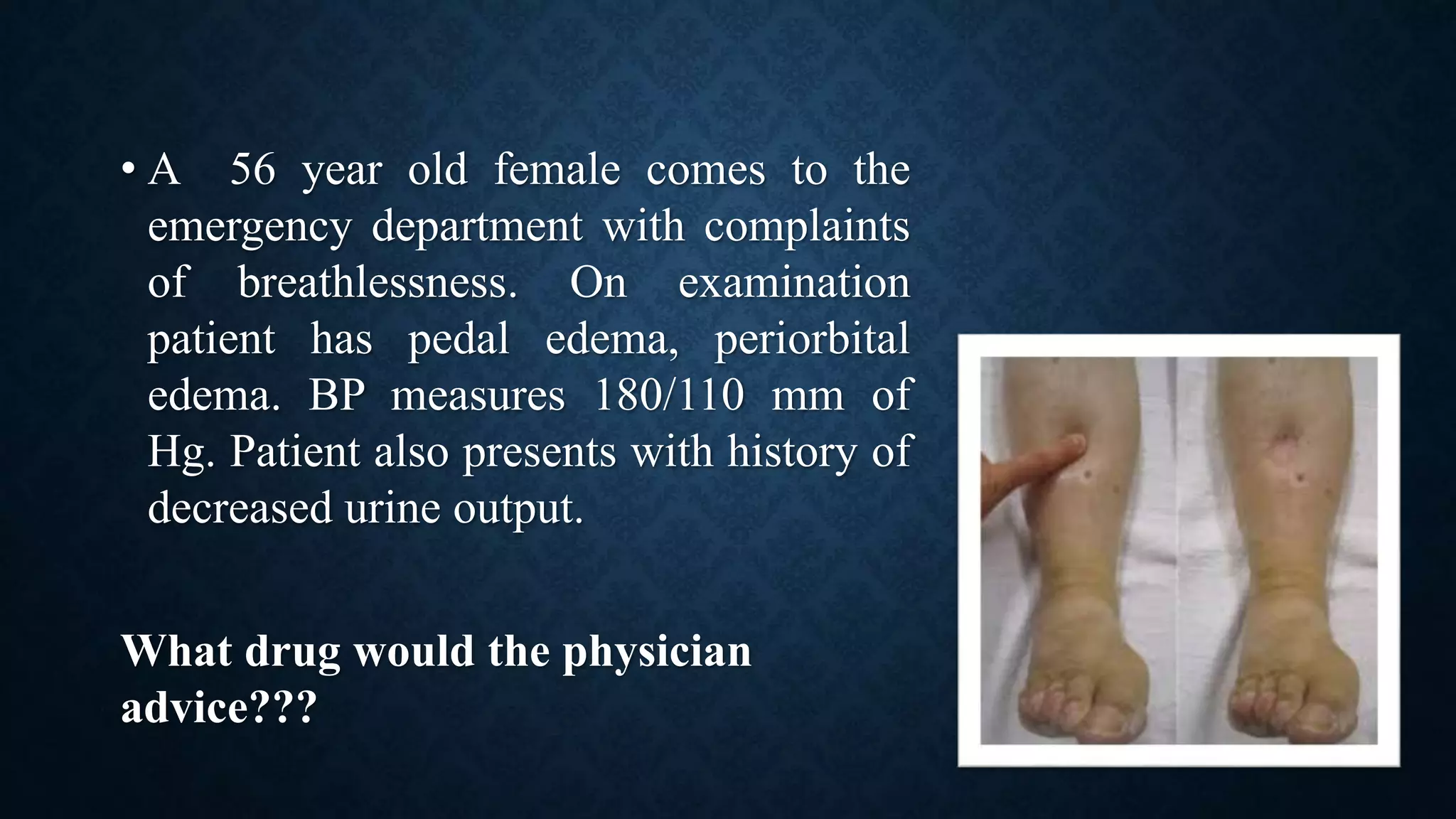
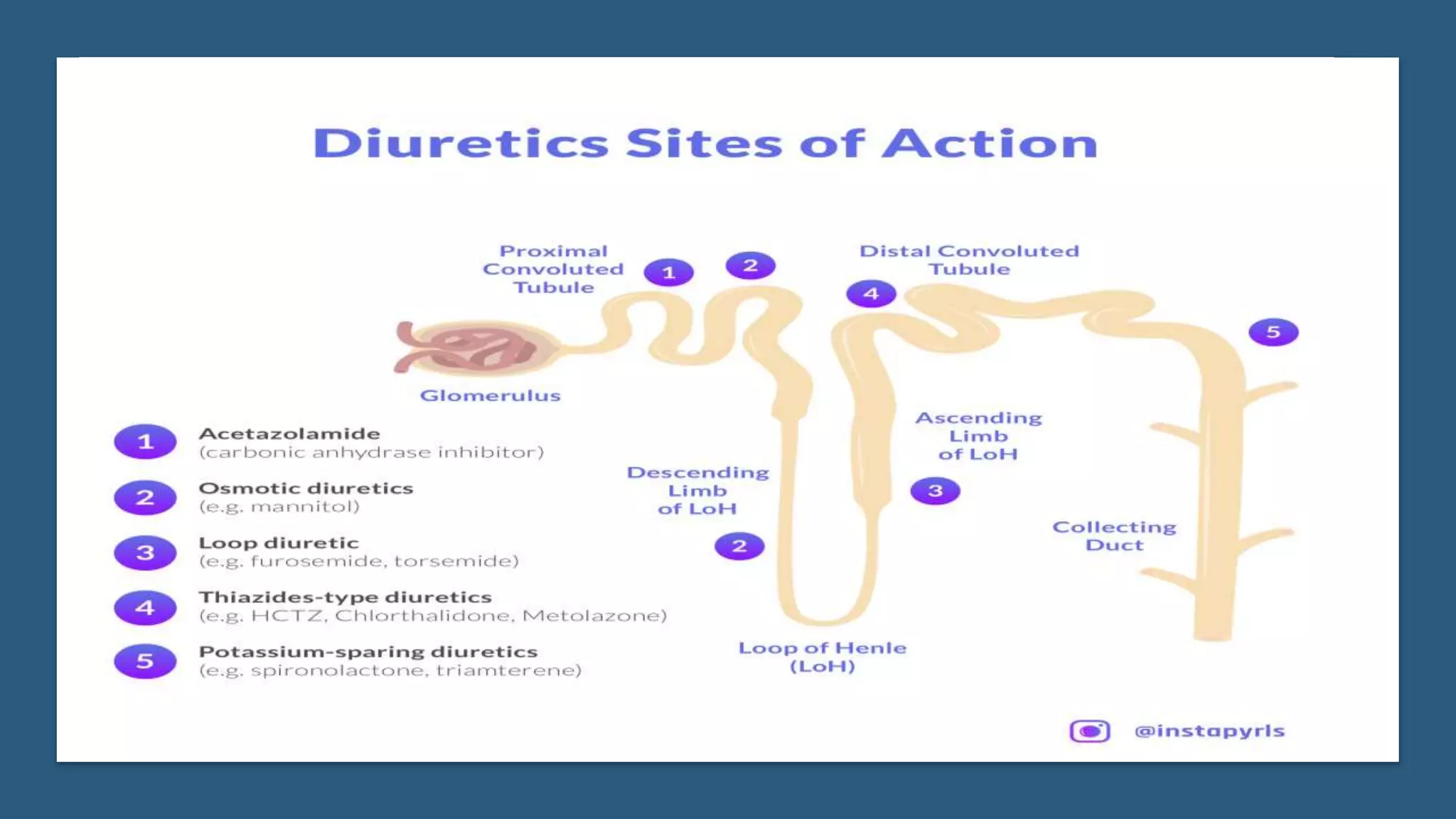
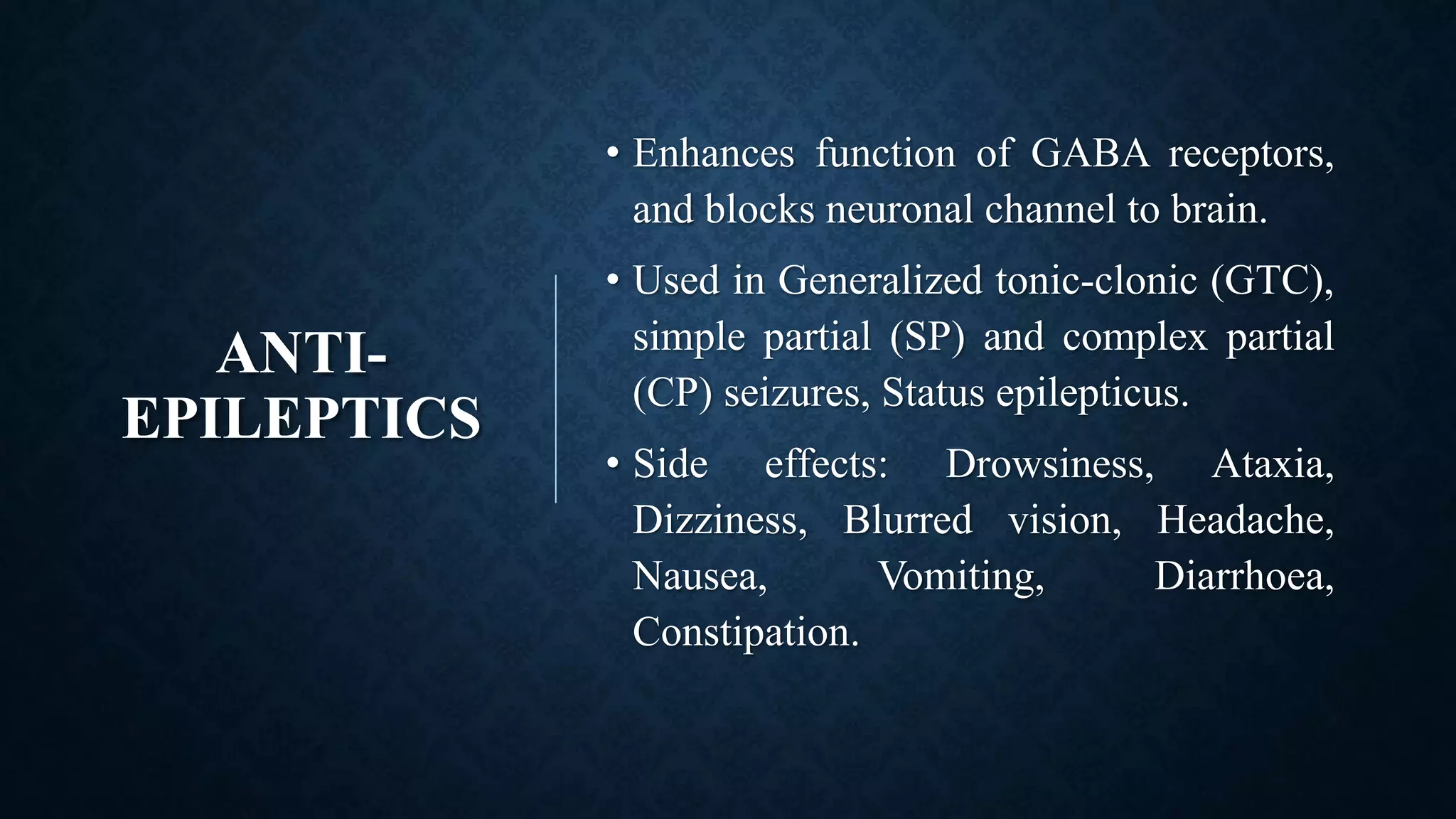
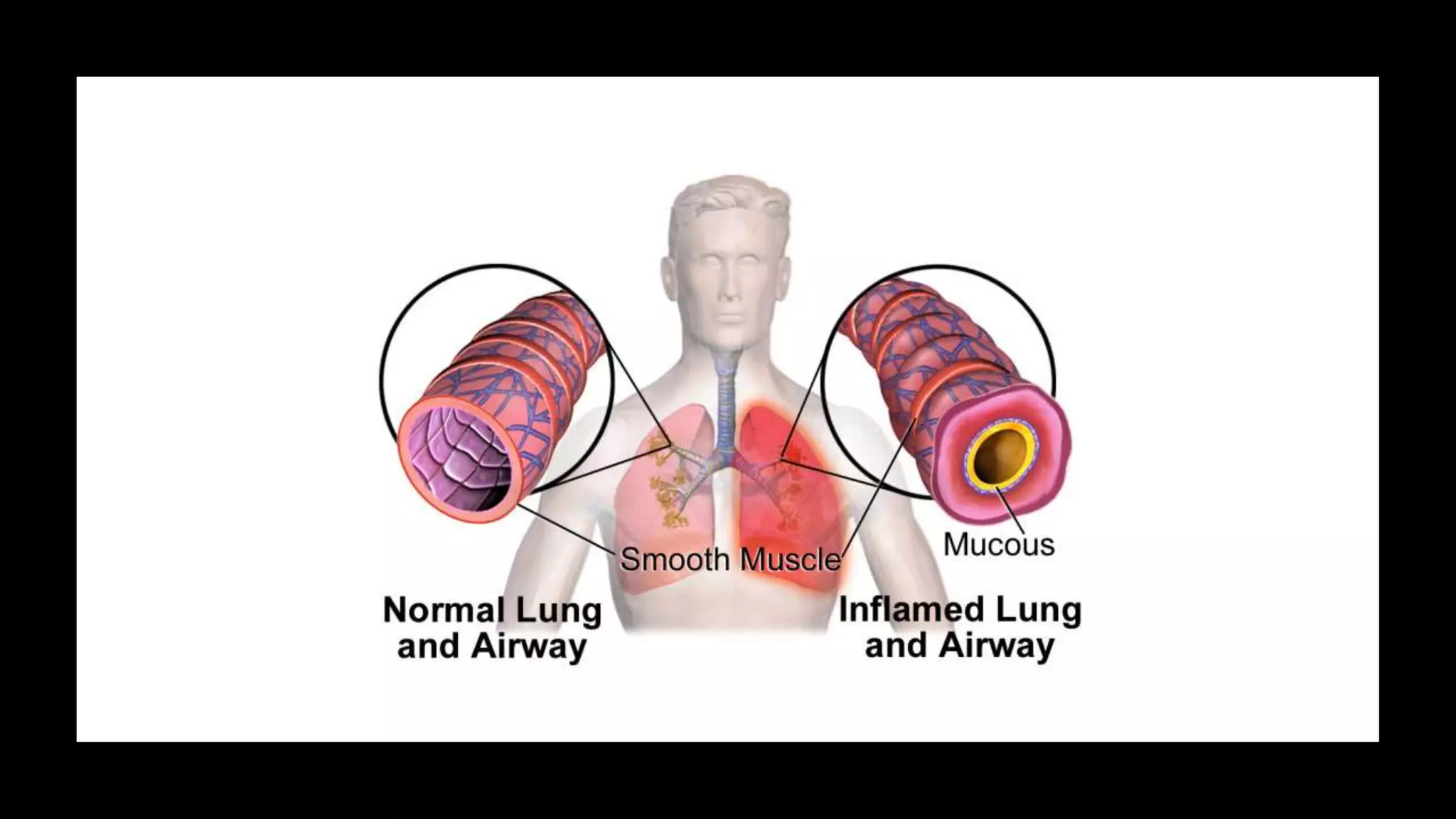
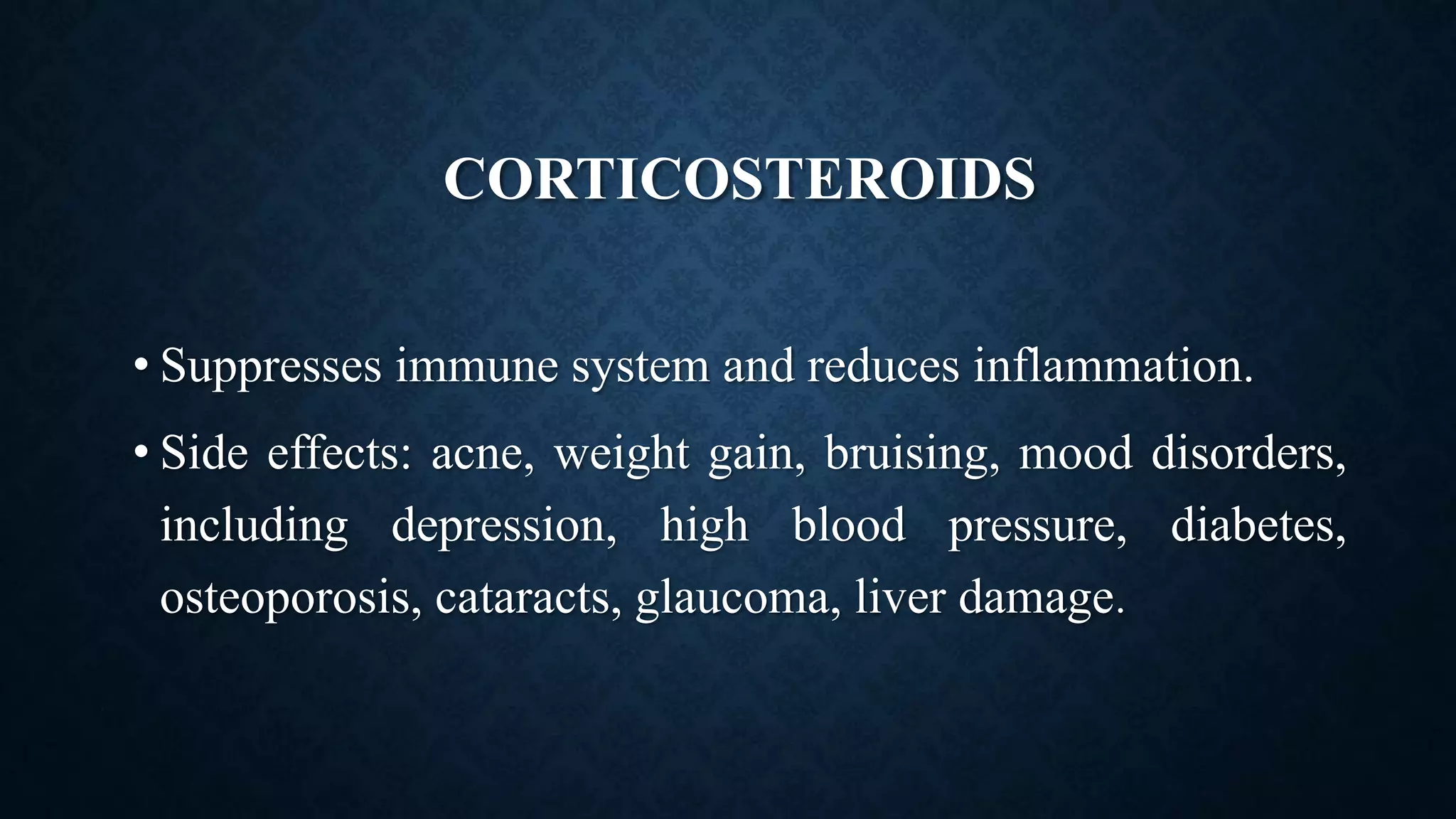
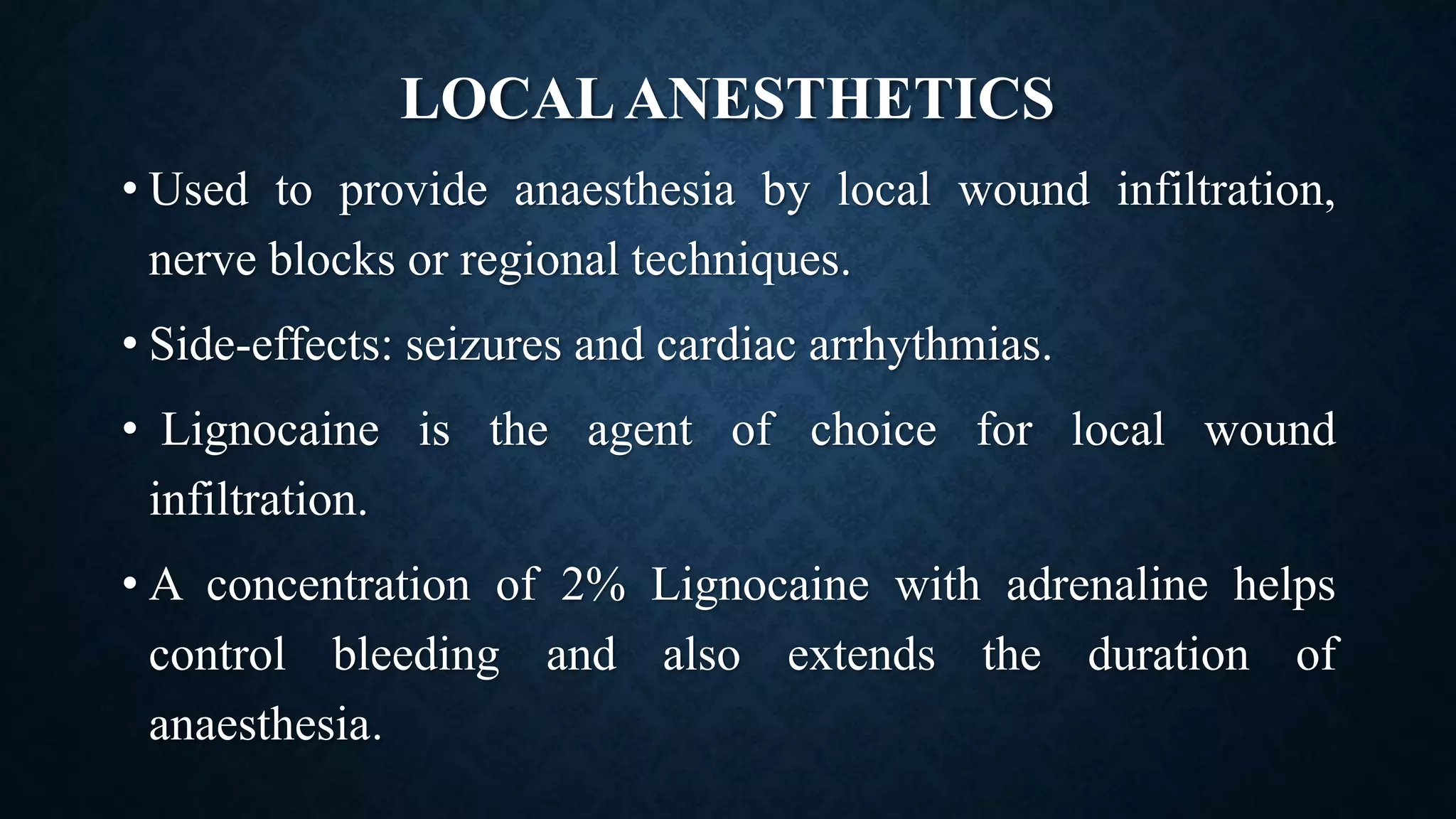
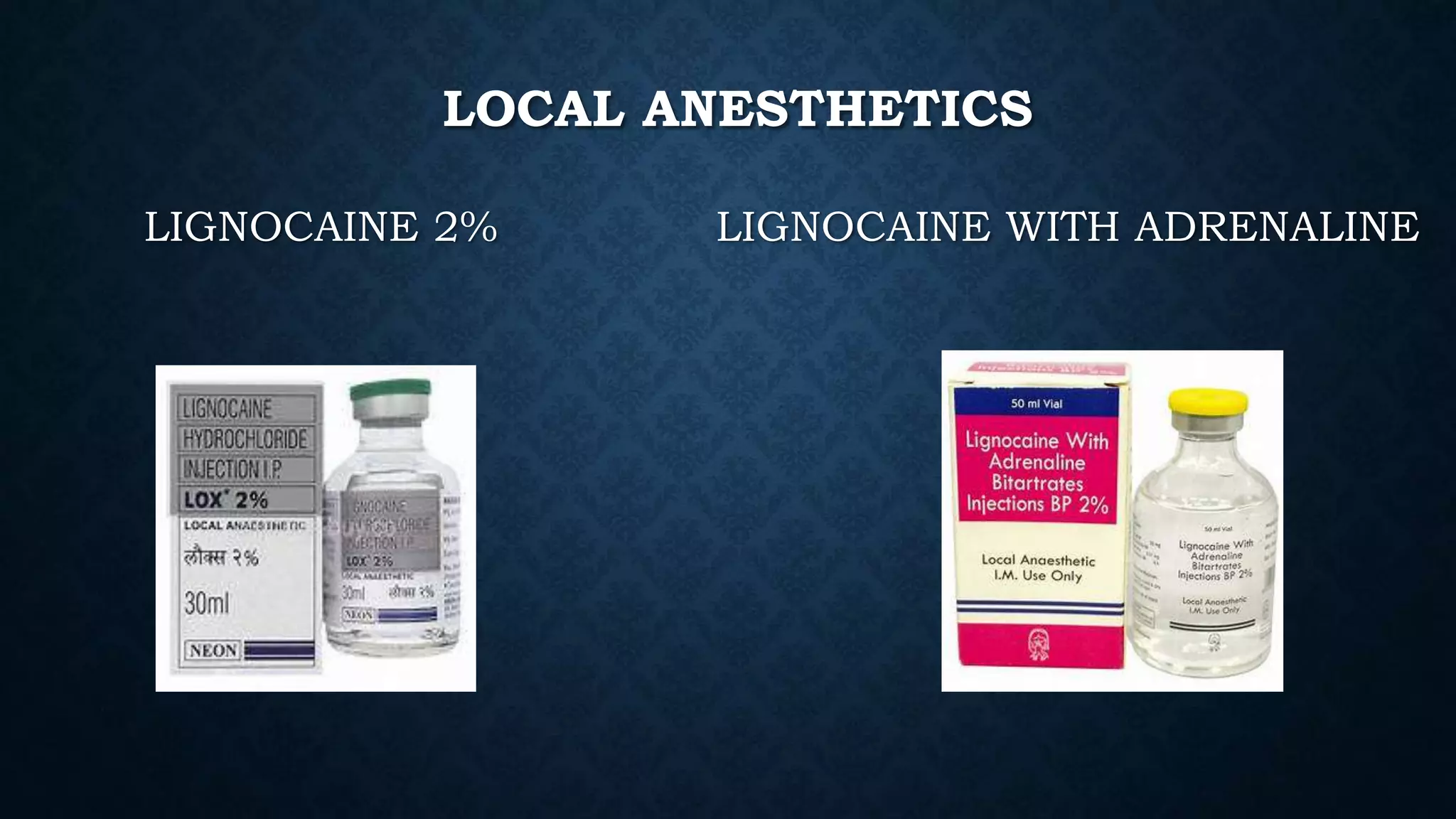
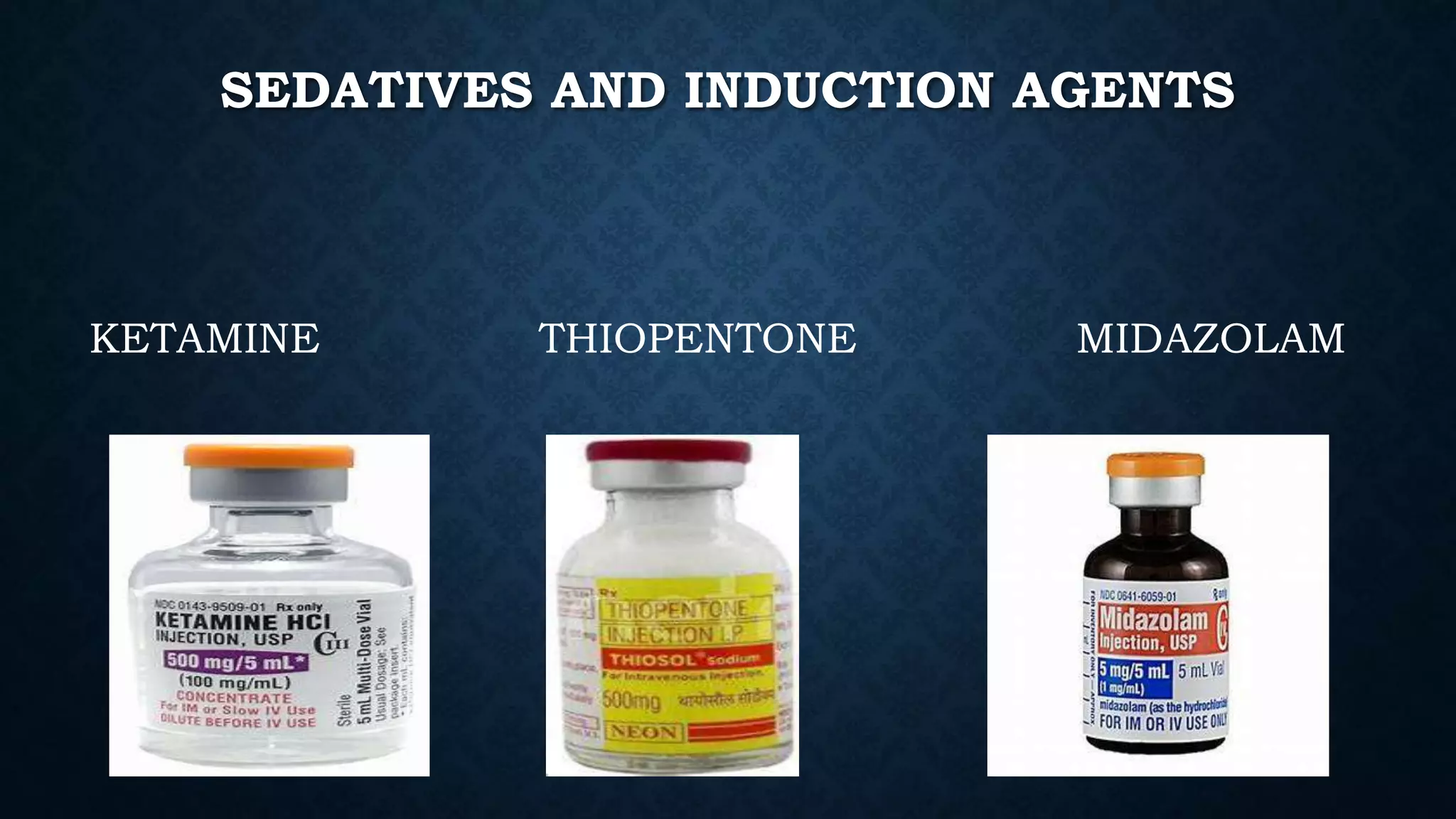
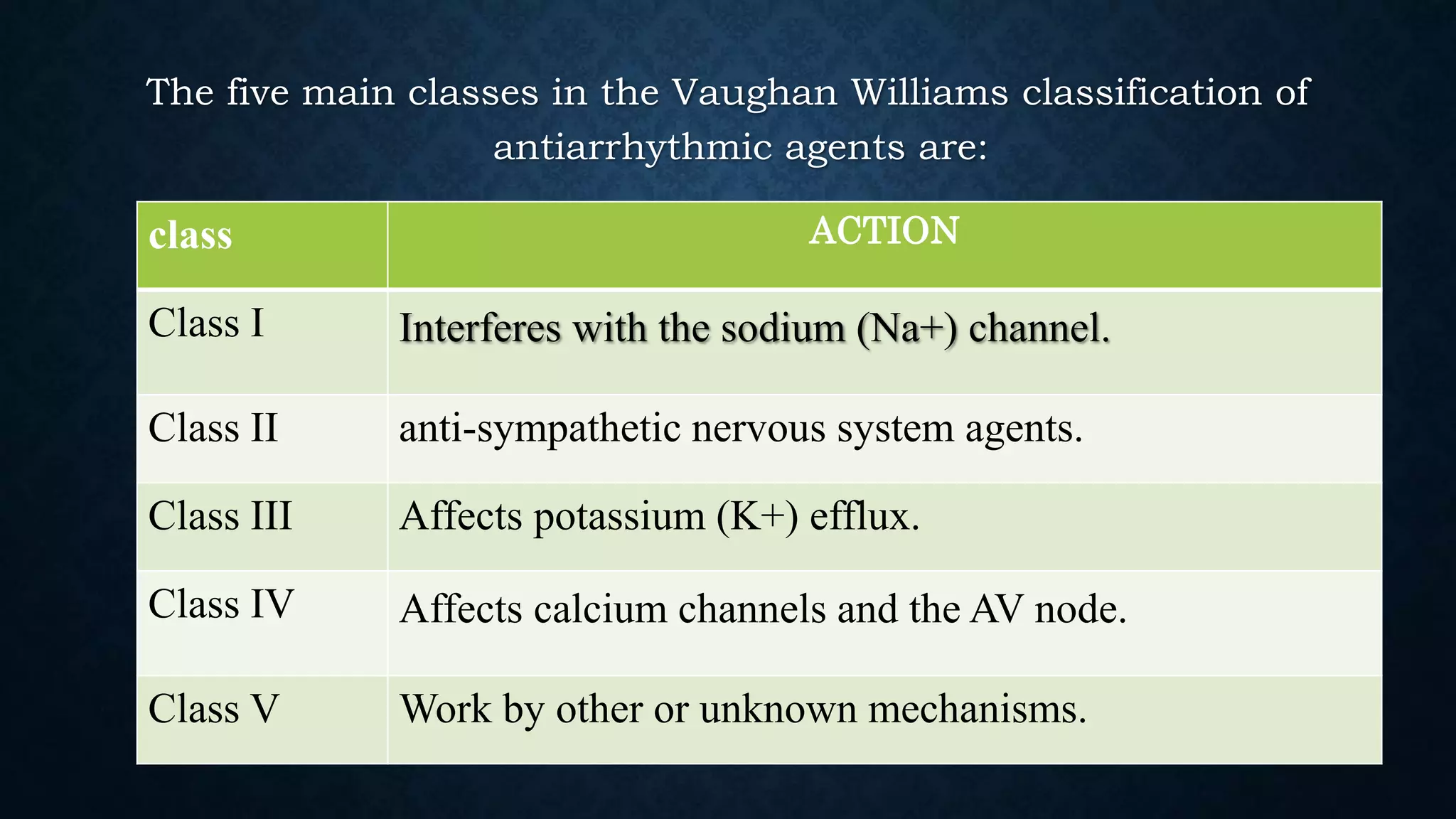
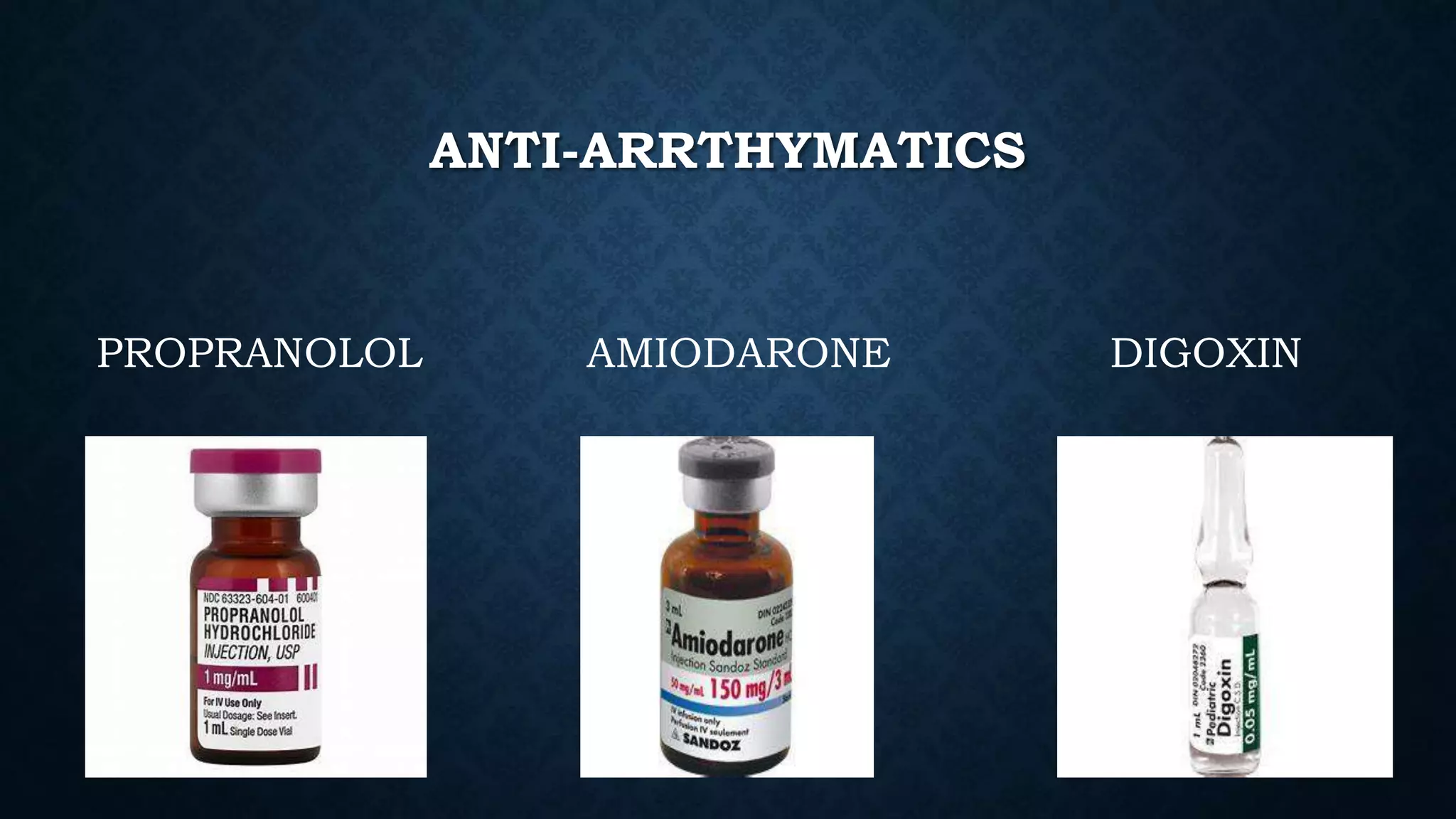
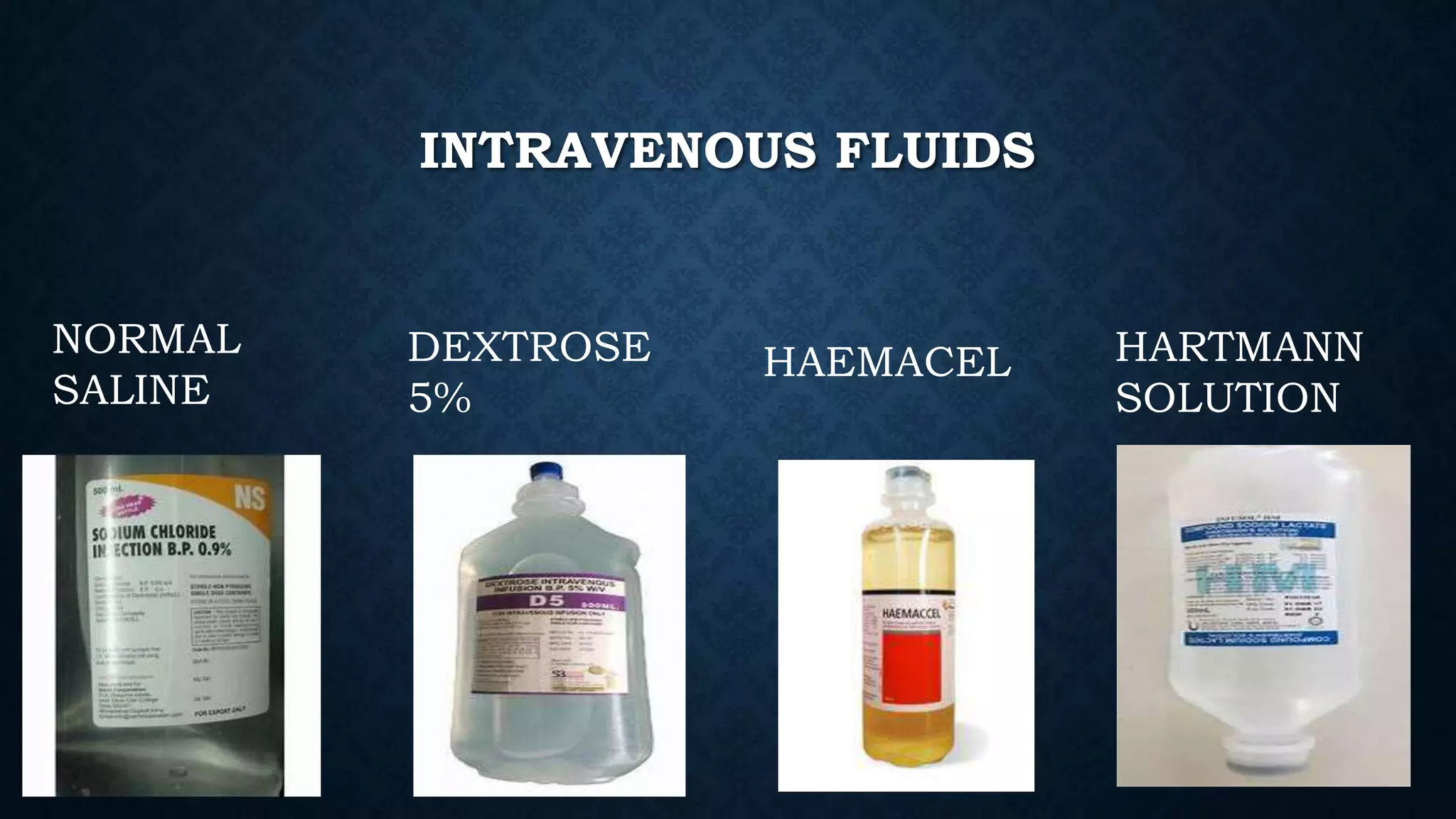
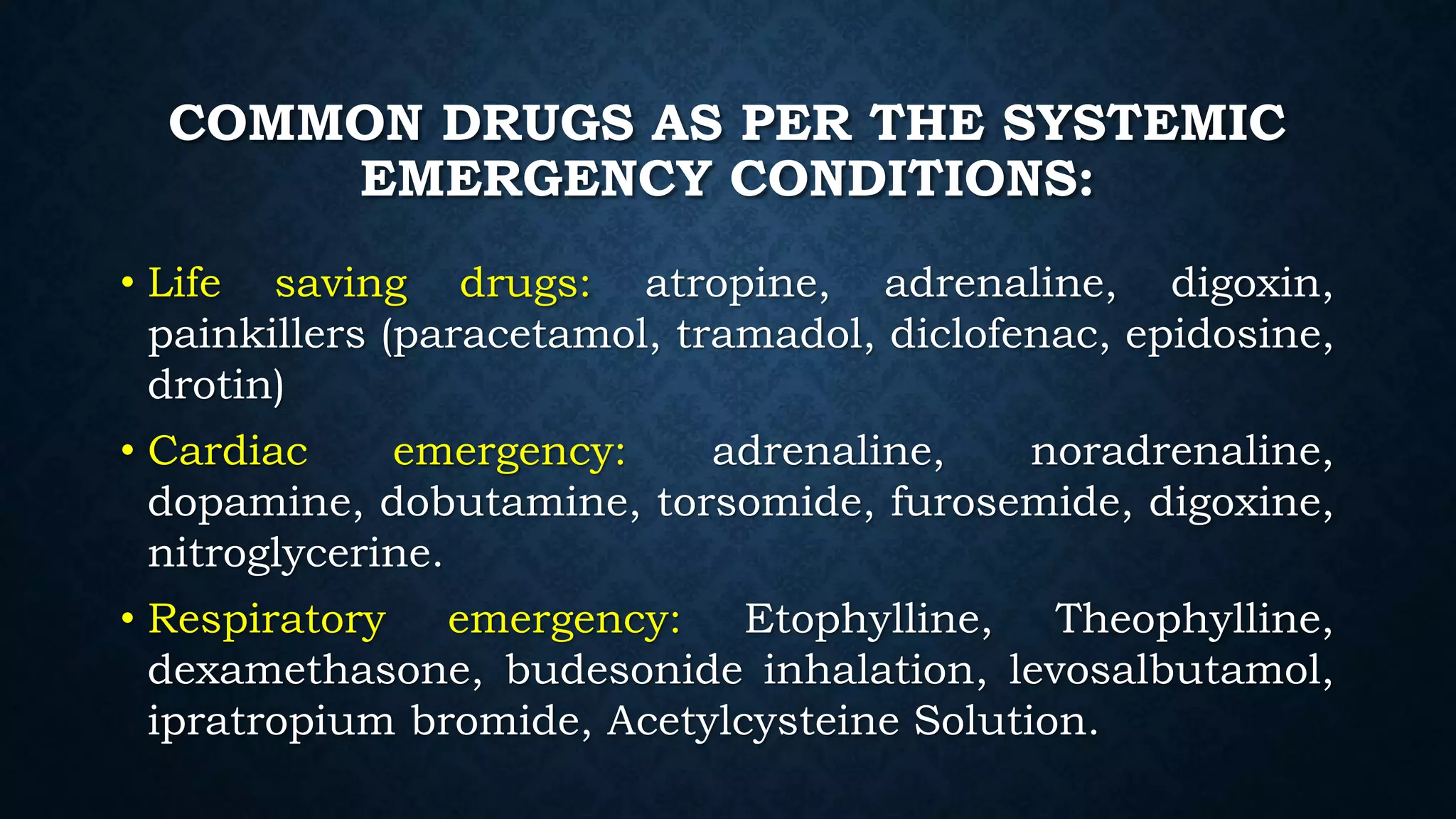
Emergency medications are used to treat life-threatening conditions and save patients' lives. They work by controlling symptoms, normalizing vital functions, and diverting patients from risks. Common categories include anti-cholinergics, inotropic agents, muscle relaxants, diuretics, anti-epileptics, neuroleptics, anti-asthmatics, corticosteroids, local anesthetics, sedatives and induction agents, opioid analgesics, anti-emetics, anti-hypertensives, anti-arrhythmics, intravenous fluids, and tetanus prophylaxis. As an emergency nurse, it is important to be familiar with these medications and their uses, dosages