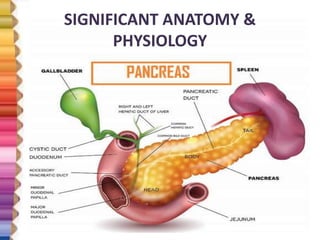
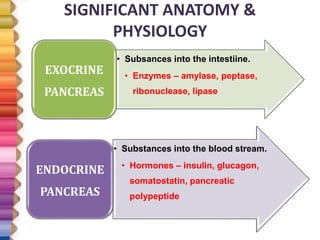
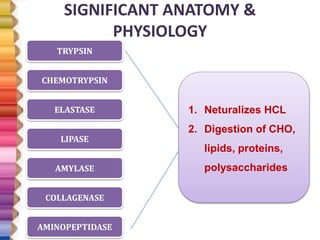
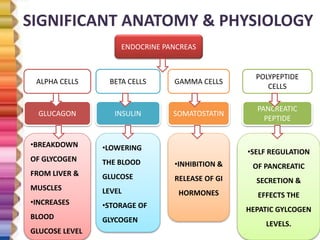
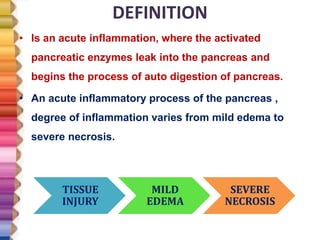
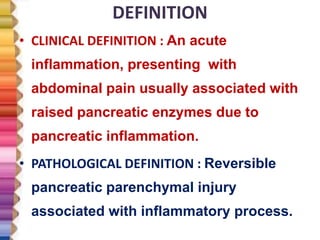
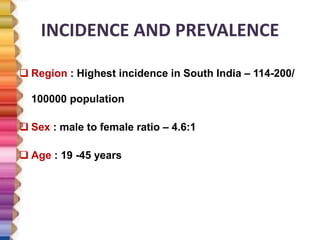
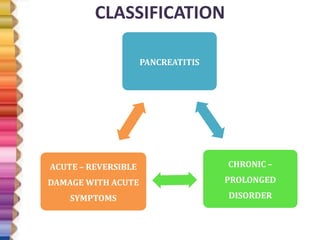
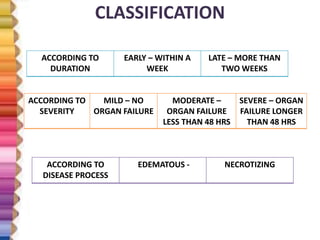
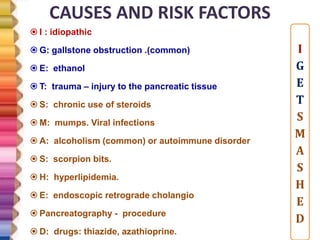
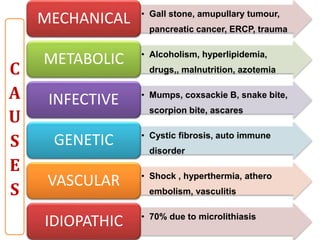
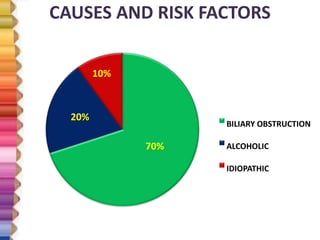
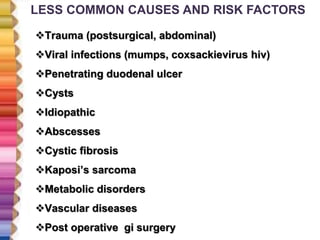
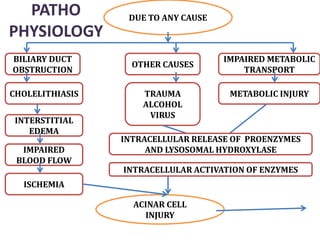
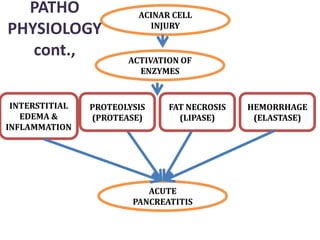
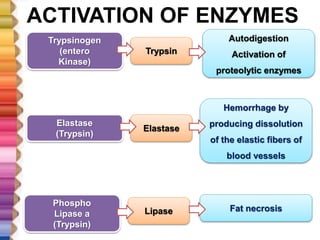
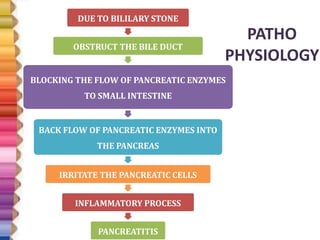
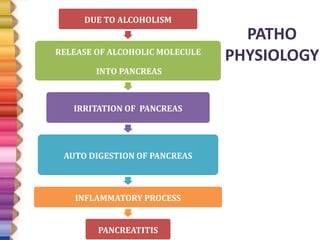
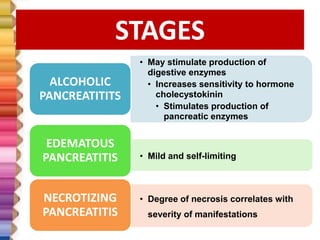
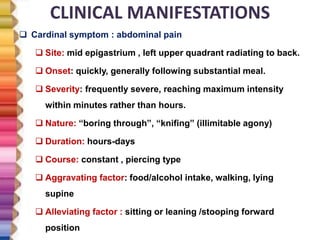
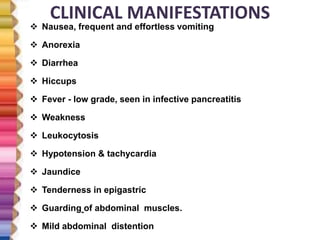
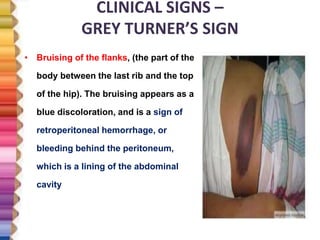
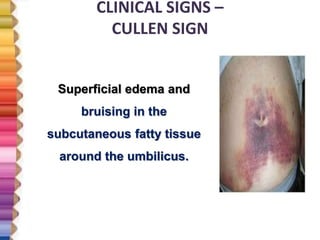
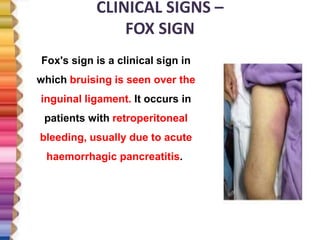
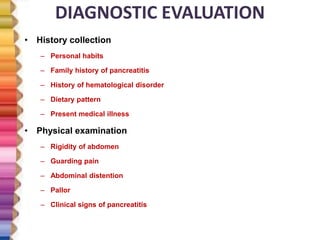
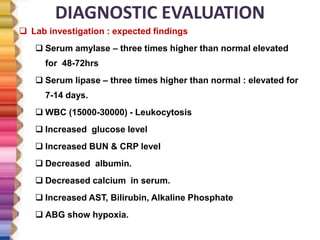
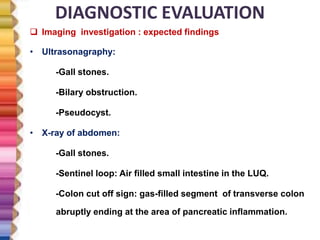
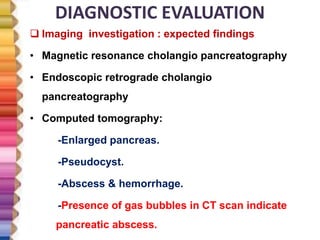
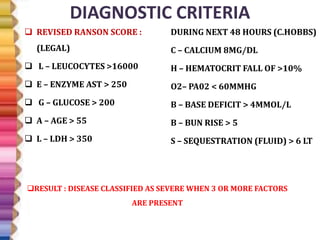
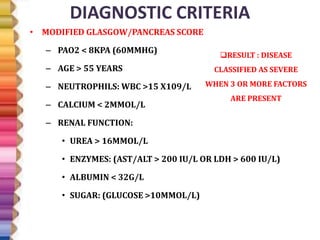
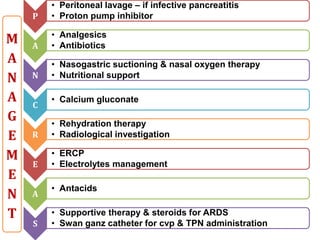
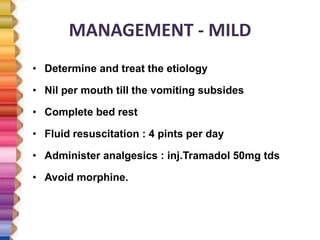
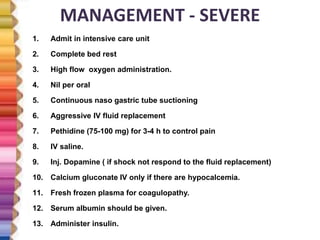
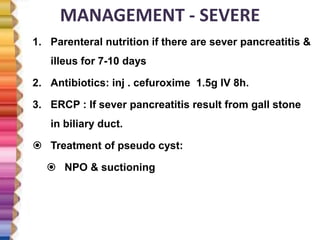
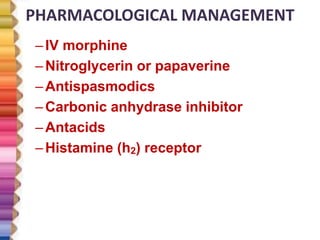
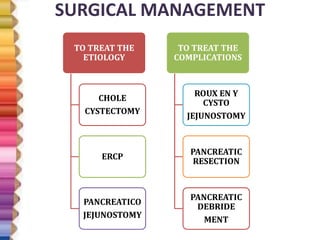
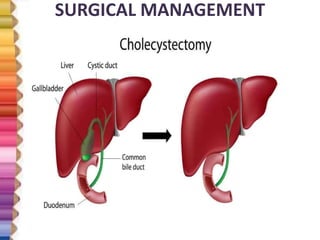
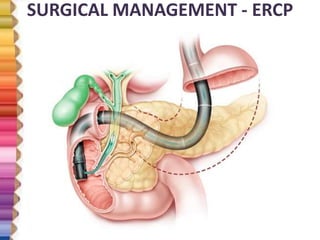
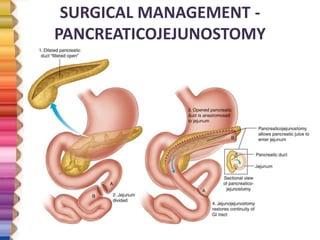
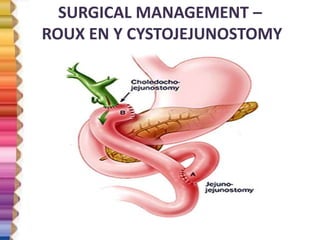
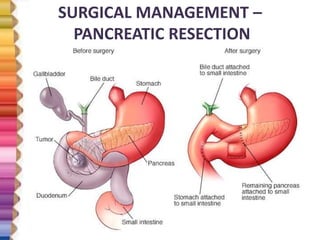
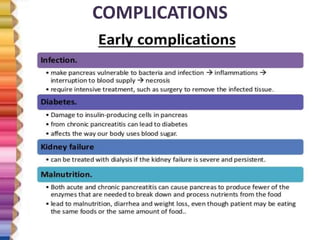
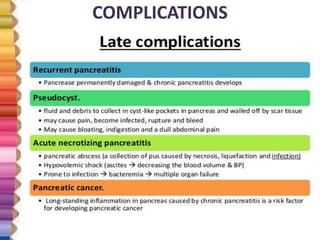
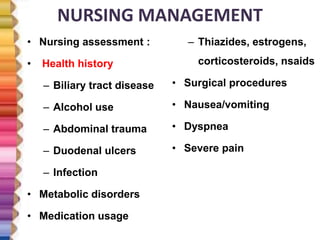
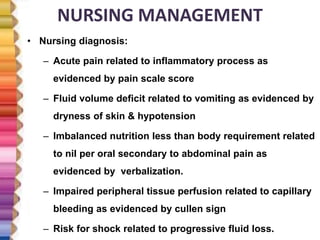
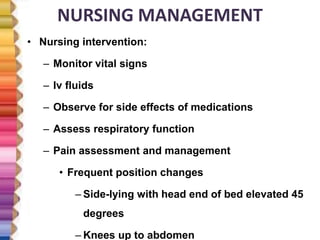
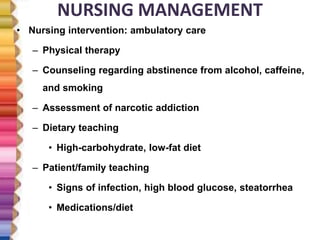
The document provides an extensive overview of pancreatitis, including its definitions, anatomy, pathophysiology, and classifications. It discusses risk factors, clinical manifestations, diagnostic evaluation techniques, and management strategies for both mild and severe cases of pancreatitis. It emphasizes the importance of early diagnosis and treatment to improve patient outcomes.