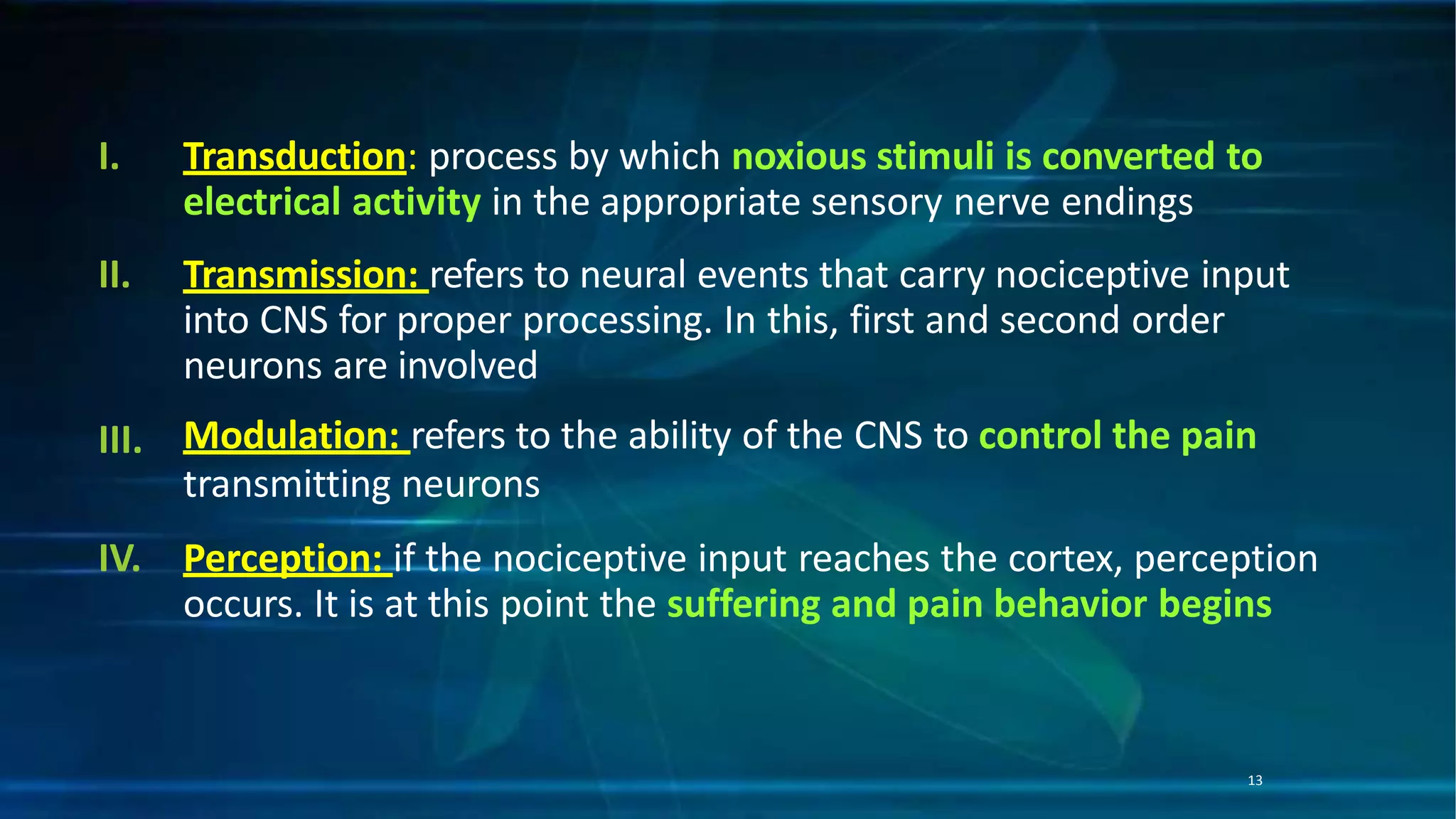
This document discusses pain control in operative dentistry. It begins with definitions of pain and classifications of pain based on duration (acute, persistent, chronic) and sensory characteristics (fast and slow pain). The neural pathways of pain and various theories of pain are described. Methods of assessing pain and factors that influence pain perception are outlined. Common causes of orofacial pain are listed along with differential diagnosis of pain. Techniques for controlling pain in restorative dentistry are provided, including local anesthesia and gaining patient confidence.