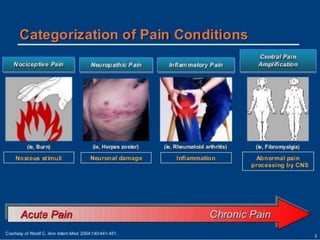
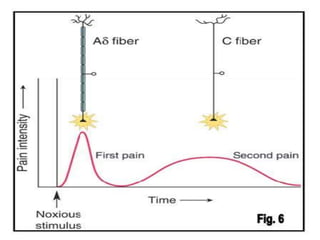
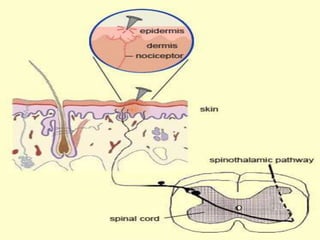
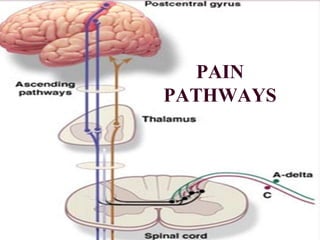
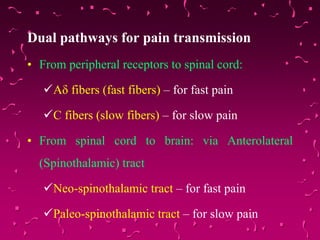
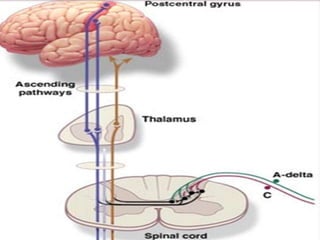
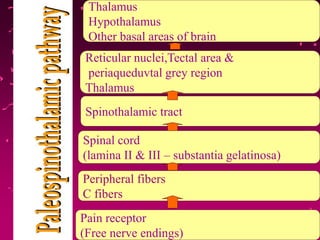
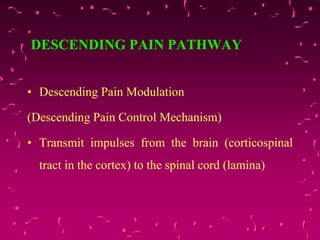
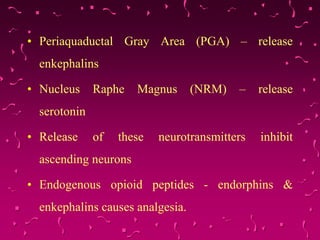
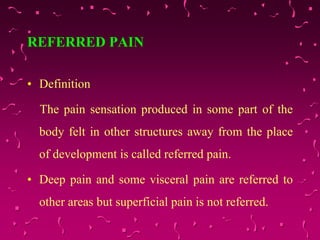
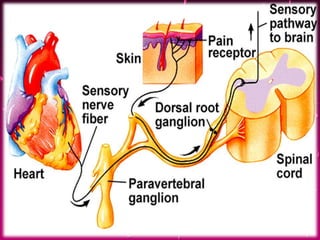
Pain is a complex experience involving sensory and emotional components. It is initiated by noxious stimuli and transmitted along specialized pain pathways in the nervous system. There are different types of pain including nociceptive, inflammatory, neuropathic, and functional pain. Pain signals are transmitted via fast Aδ fibers and slow C fibers from receptors to the spinal cord and then to the brain. The transmission of pain can be modulated by descending pathways and inhibited using various pharmacological and surgical techniques. Managing pain involves understanding its underlying causes and mechanisms.