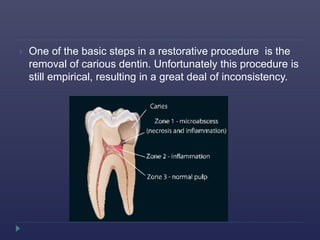
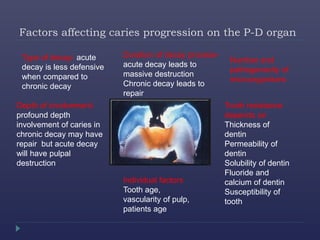
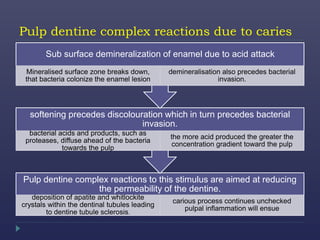
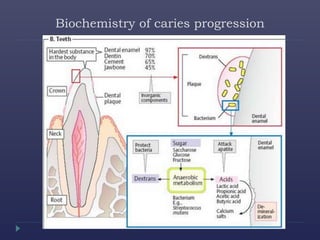
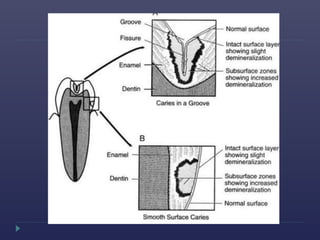
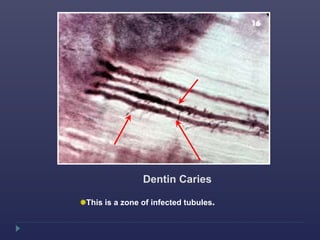
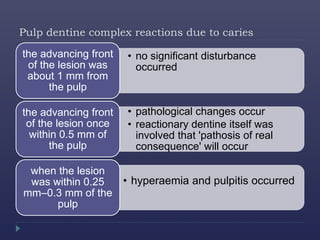
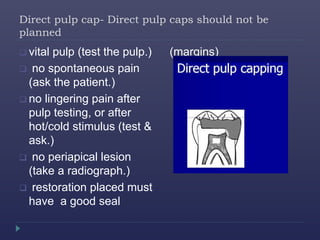
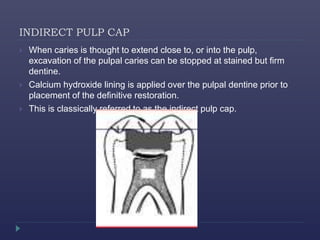
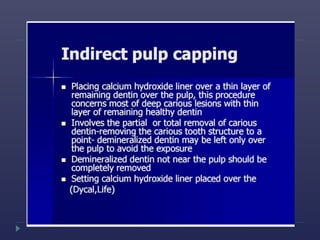
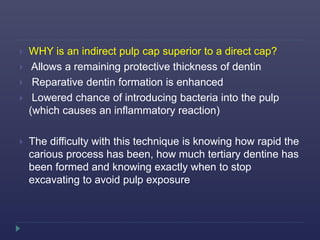
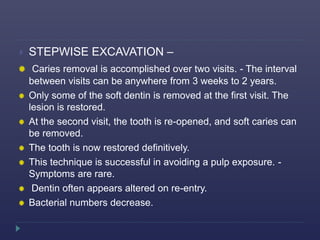
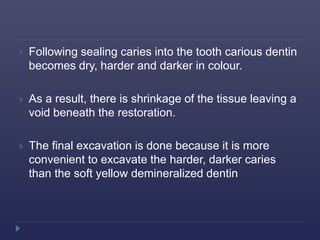
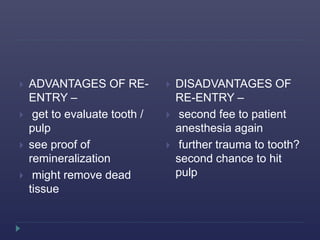
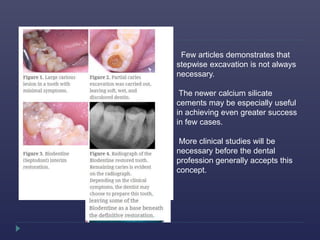
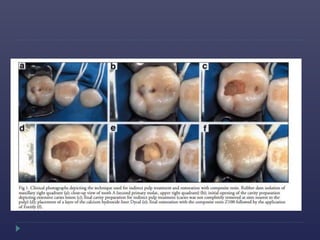
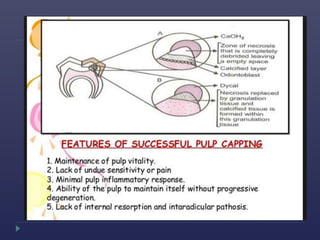
The document discusses the complexities of managing deep carious lesions in dentistry, emphasizing the importance of accurately diagnosing and treating them to prevent pulpal damage. It outlines various techniques such as direct and indirect pulp capping, detailing their indications, materials used, and the challenges faced, including the decision-making process in caries excavation. The effectiveness of different treatments and the need for further clinical studies on newer materials like calcium silicate cements are also highlighted.