This document discusses ceramic laminate veneers, including:
- Their history and evolution from thin plastic facings bonded in the 1930s to modern ceramic laminates.
- Definitions of terms like porcelain laminate veneer and laminating.
- Indications and contraindications for ceramic laminate veneers.
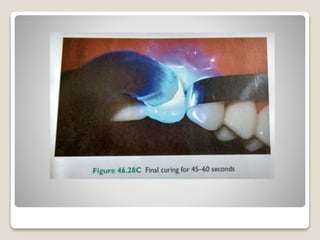
- Details of the tooth preparation process, including types of preparations, instrumentation used, and steps like labial reduction and incisal coverage.
- The importance of shade selection, soft tissue management, and impression techniques.