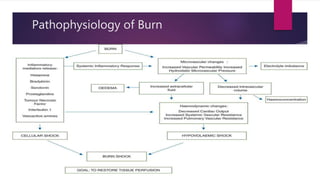
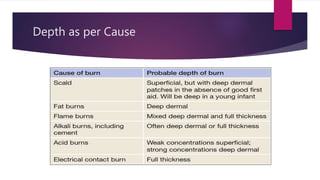
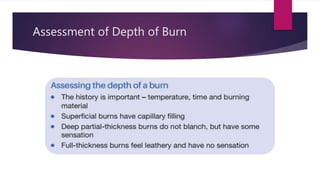
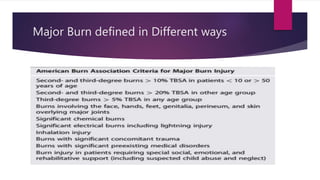
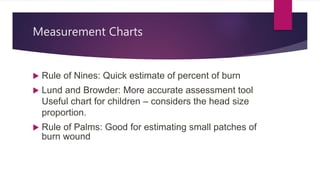
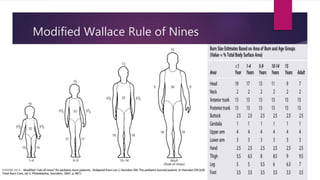
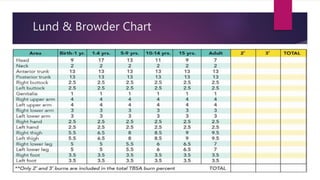
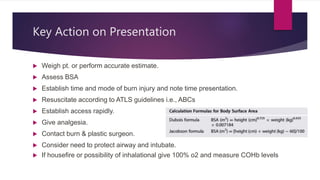
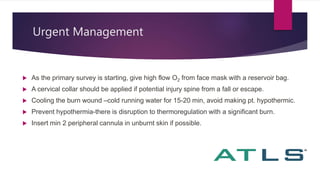
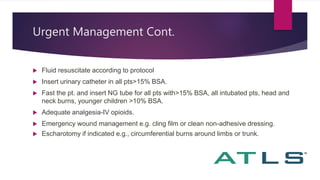
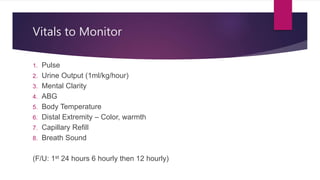
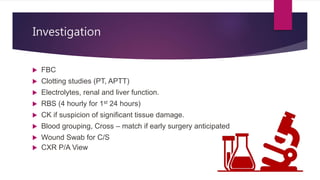
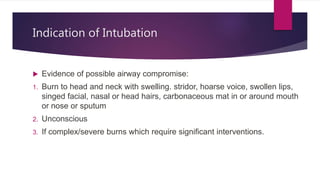
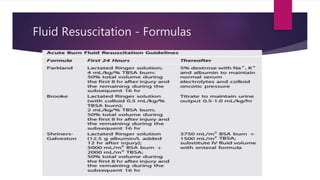
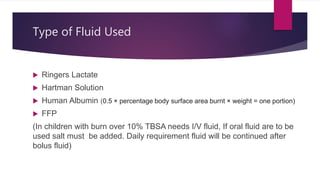
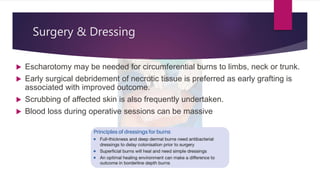
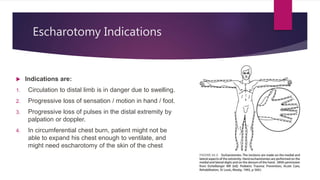
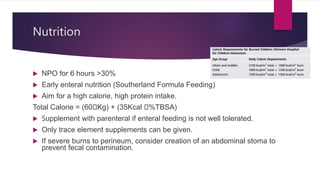
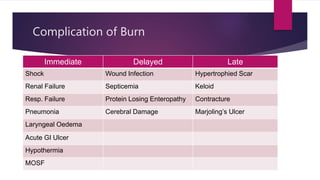
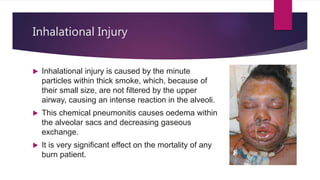
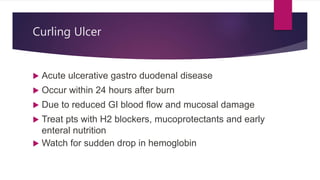
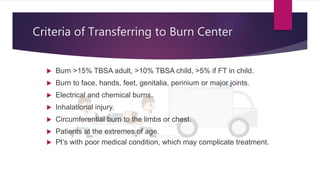
The document presents a comprehensive overview of burn management in children, detailing the causes, assessment, and urgent management practices necessary for treating burns, which typically account for 6% of pediatric injuries. Key points include the importance of fluid resuscitation, monitoring vital signs, and considering the size and depth of burns to guide treatment. It also discusses surgical interventions, wound management strategies, and rehabilitation to ensure optimal recovery outcomes for pediatric patients.