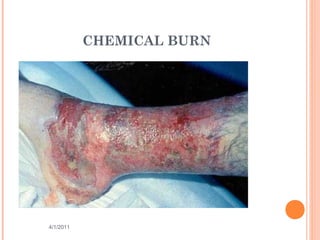
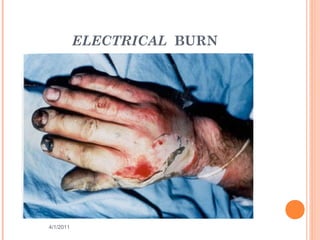
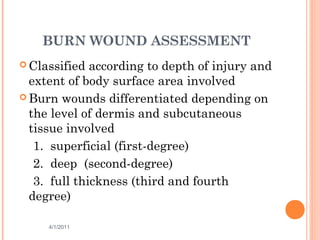
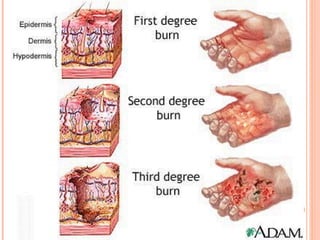
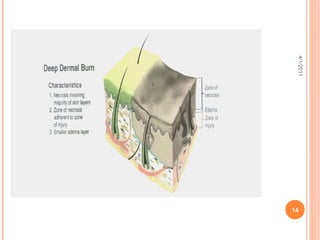
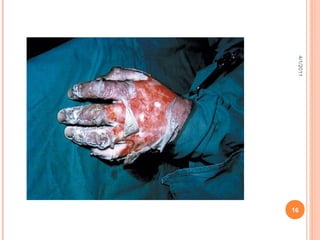
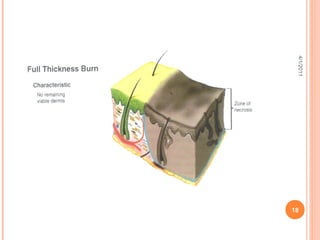
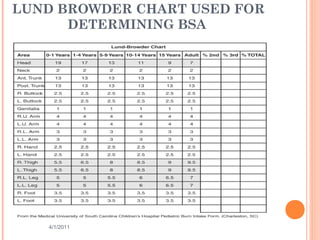
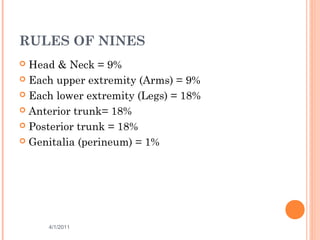
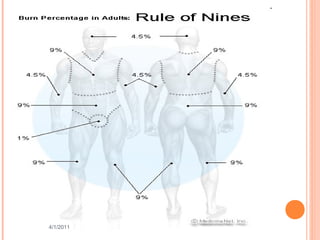
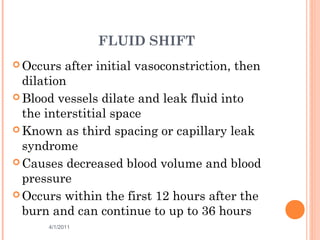
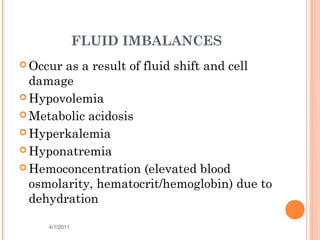
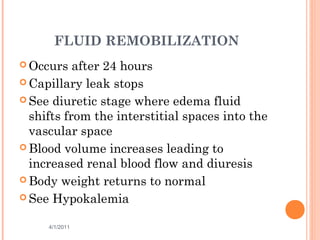
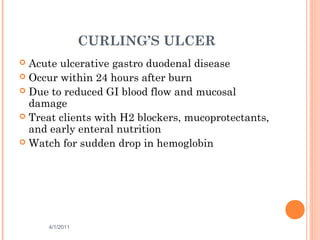
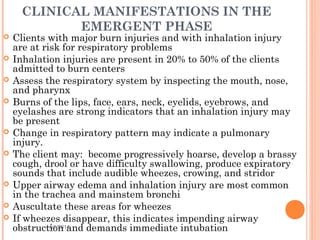
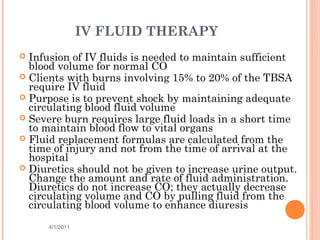
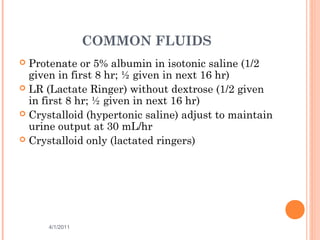
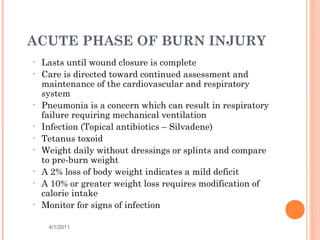
The document provides comprehensive information on burn injuries, their types, management, and phases of treatment including the emergent, acute, and rehabilitative stages. It outlines the classification of burns based on depth and body surface area, assessment techniques, complications such as fluid shifts, and necessary interventions such as fluid resuscitation and infection prevention. Various nursing diagnoses relevant to each phase of treatment are also discussed, along with the importance of ongoing evaluation and psychosocial support for recovery.