- A 11-year-old girl presented with a 1% second degree burn on her right hand after accidentally dipping it in hot porridge.
- She was initially treated with topical creams but referred to the hospital due to worsening symptoms.
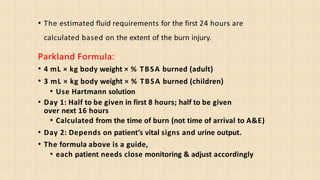
- In the hospital she received IV fluids, antibiotics, and wound dressing changes. Her burn wound was cleaned and exposed dermis covered.
- Her condition improved with treatment and she was discharged with oral antibiotics and follow-up appointments. At her follow-up her wound had fully healed.