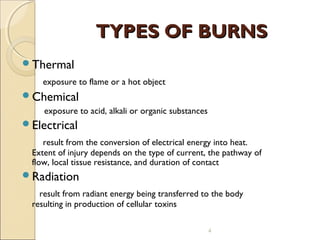
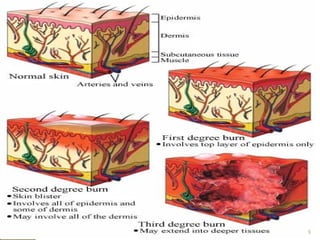
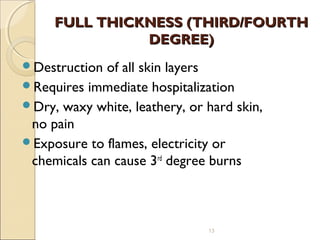
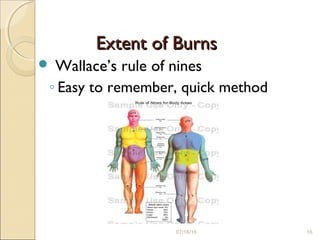
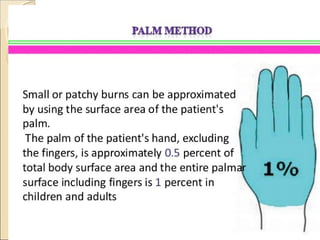
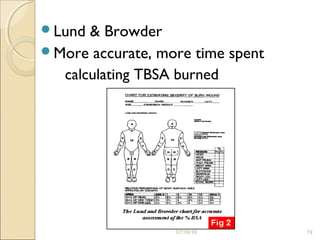
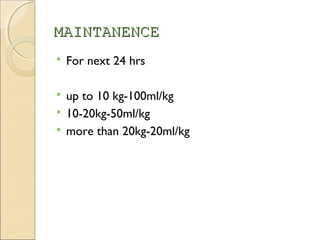
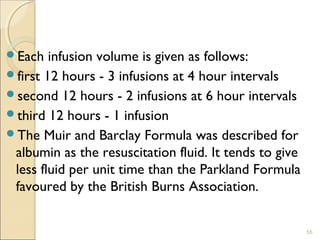
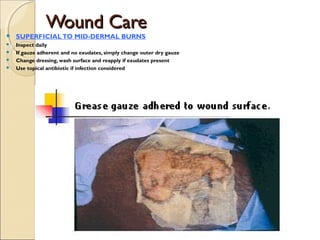
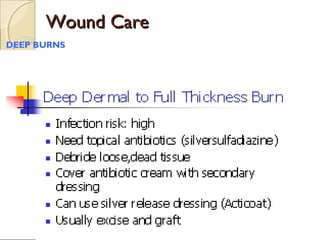
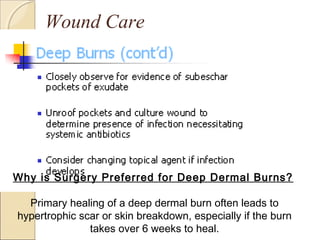
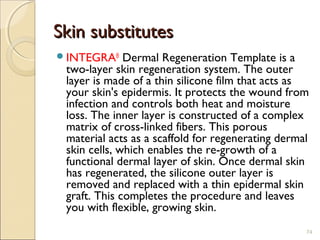
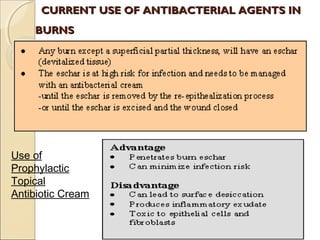
This document provides information on the pathophysiology and treatment of burns. It discusses the local and systemic effects of burns including cardiovascular, renal, pulmonary, gastrointestinal and immune responses. It describes methods of assessing burn severity including depth of burn and percentage of total body surface area burned. Treatment involves fluid resuscitation according to the Parkland formula, wound care, infection control, nutrition and management of complications like multiorgan failure.