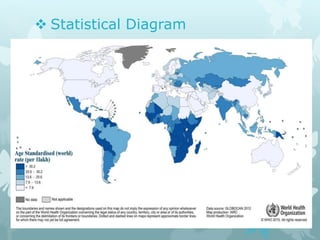
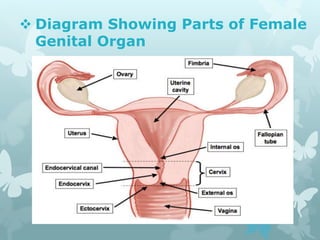
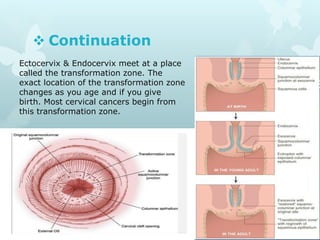
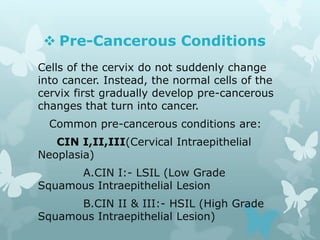
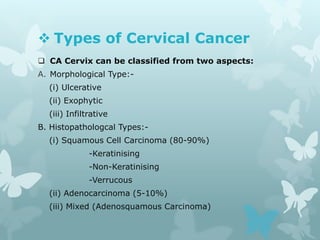
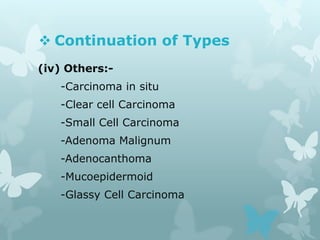
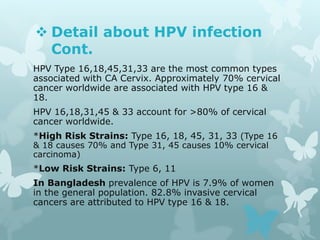
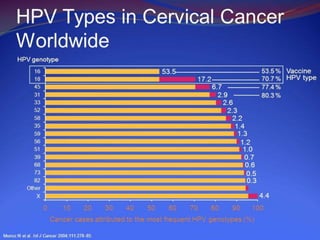
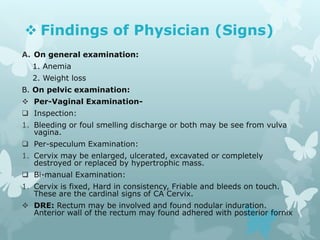
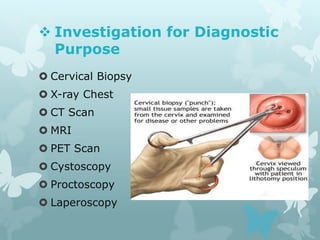
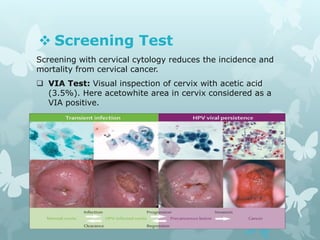
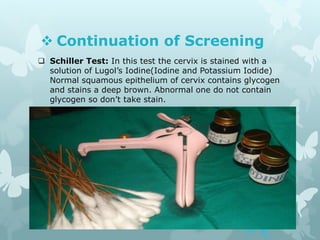
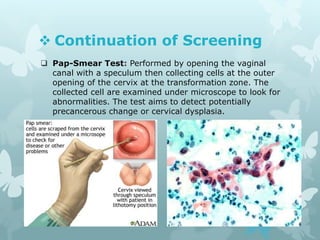
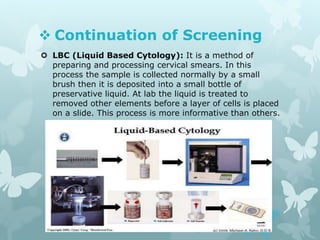
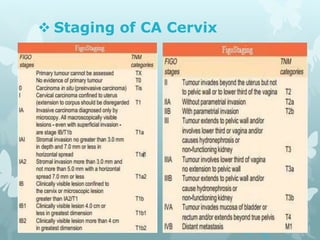
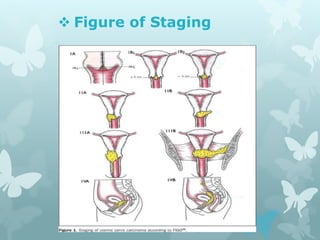
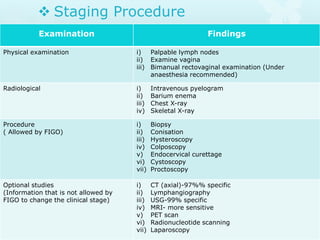
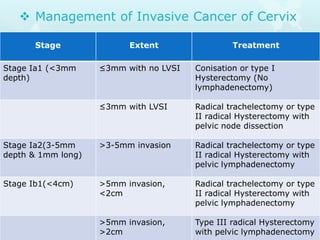
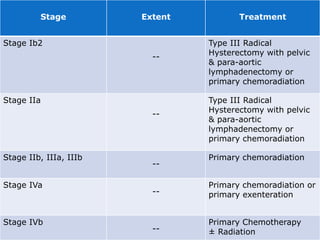
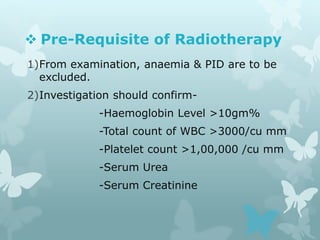
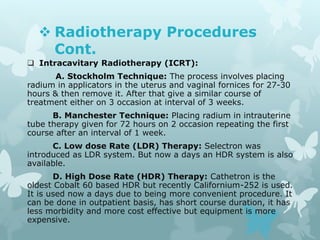
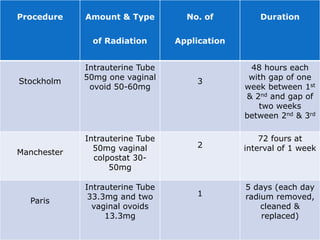
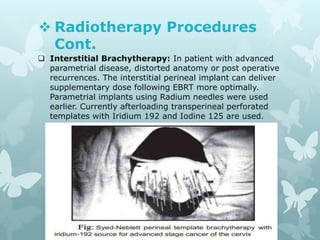
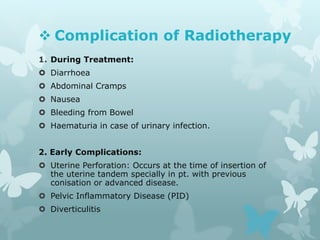
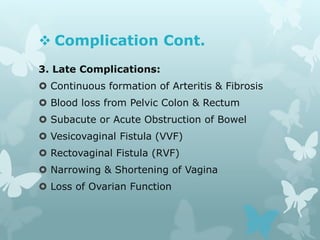
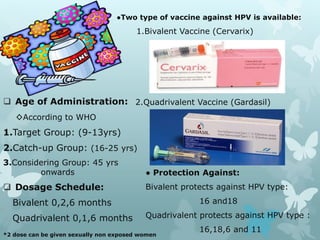
This document provides information about a seminar on cervical cancer. It begins with an introduction explaining why cervical cancer awareness is important as it is a common and deadly form of cancer for women worldwide. Statistics about the incidence and mortality of cervical cancer globally and in Bangladesh are then presented. The document goes on to describe cervical cancer itself, including risk factors, types, staging, symptoms, diagnostic testing, and treatment options such as surgery, radiation therapy, and chemotherapy. Pre-requisites for radiation therapy and different radiotherapy procedures are outlined. The goal of the summary is to highlight the key topics covered in the document at a high level in 3 sentences or less.