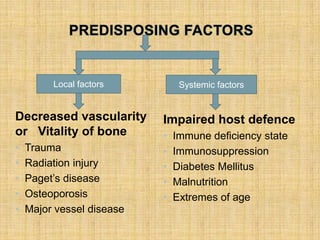
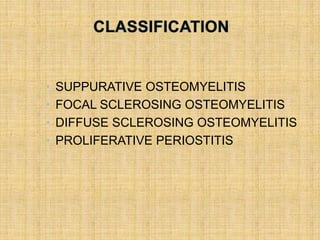
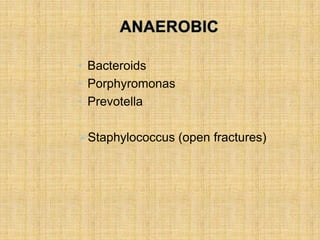
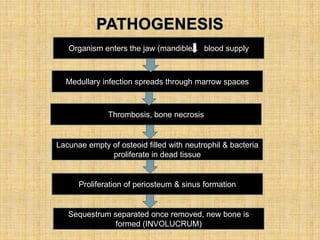
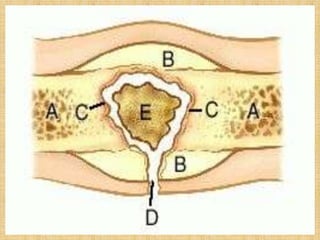
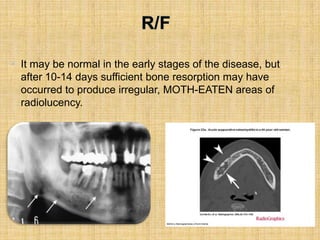
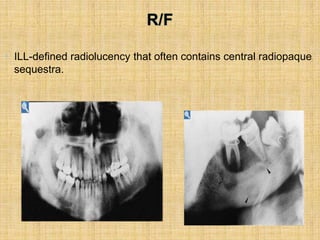
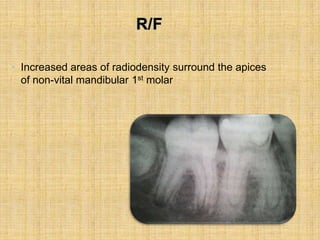
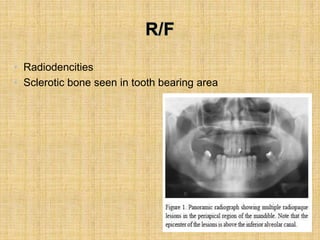
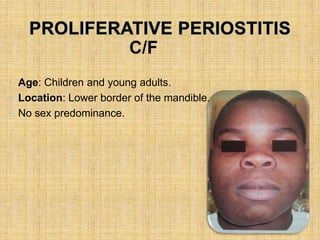
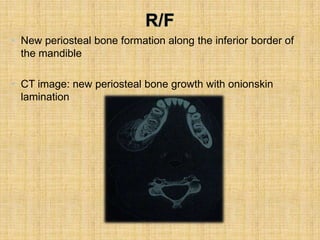
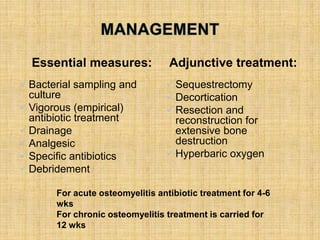
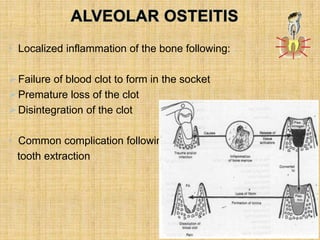
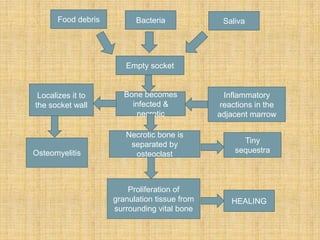
This document discusses osteomyelitis and alveolar osteitis. It defines osteomyelitis as an inflammatory process in the bone marrow or cortical surfaces that extends from the initial site of involvement. It then discusses predisposing factors, classifications, clinical features, radiographic features, and management of osteomyelitis. It also defines alveolar osteitis as localized inflammation of the bone following failure of a blood clot or socket, discusses its pathogenesis and clinical features, and outlines its treatment.