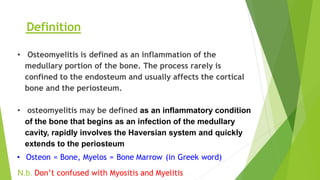
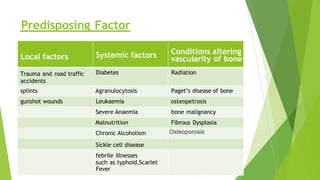
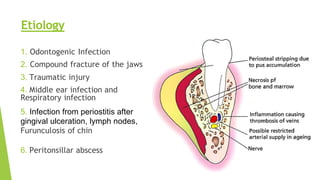
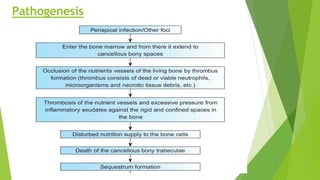
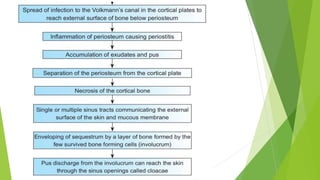
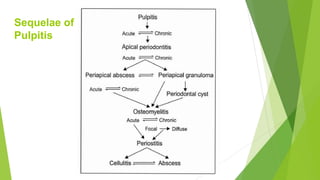
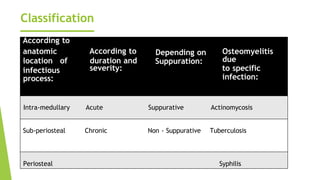
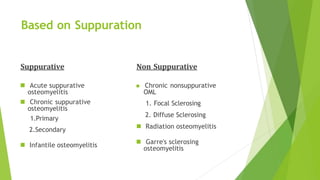
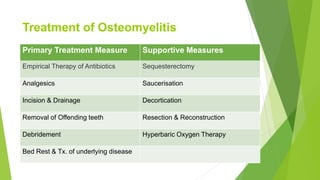
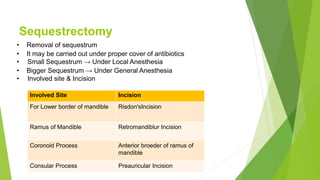
Osteomyelitis is an inflammation of the bone marrow that begins as an infection in the medullary cavity and spreads to involve the bone and periosteum. It can be caused by local trauma, systemic conditions like diabetes that impair blood flow, or infections from other sites like the teeth, middle ear, or lungs. Symptoms include pain, swelling, fever. It is classified based on duration (acute vs chronic), presence of pus (suppurative vs non-suppurative), location in bone, and specific causative infection. Treatment involves antibiotics, removal of infected or dead bone, drainage of pus, and sometimes surgery.