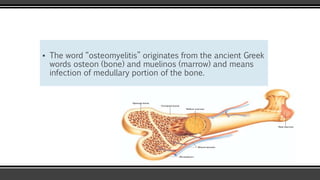
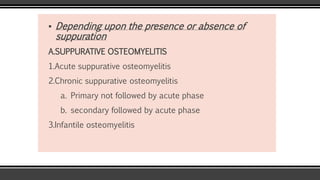
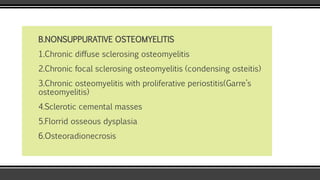
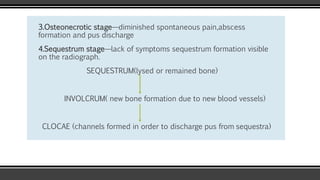
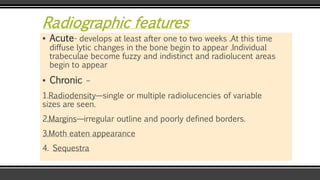
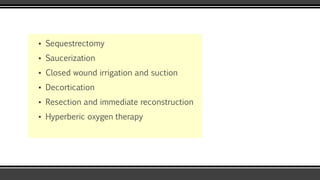
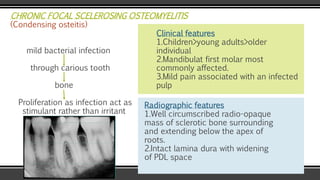
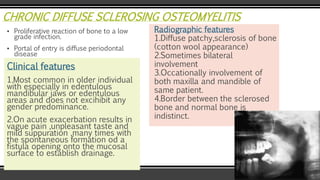
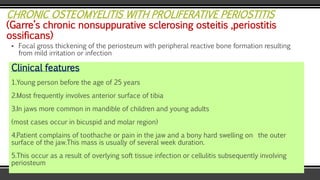
The document discusses osteomyelitis of the jaws, detailing its definitions, classifications, pathogenesis, clinical features, diagnostic methods, and management strategies. It outlines different forms of osteomyelitis, including acute and chronic variations, as well as their clinical presentations, radiographic features, and predisposing factors. Management focuses on eradicating infection, which may include surgical interventions, antibiotic therapy, and supportive care.